Has only a somatic motor (general somatic efferent) component.
Somatic motor: innervates the lateral rectus muscle of the ipsilateral orbit.
The lateral rectus muscle is one of the six extraocular muscles responsible for the precise movement of the eye for visual tracking or fixation on an object.
See the CN III section (occulomotor nerve) for a discussion of eye movements and the interaction between the three nuclei and nerves that innervate the extraocular muscles.
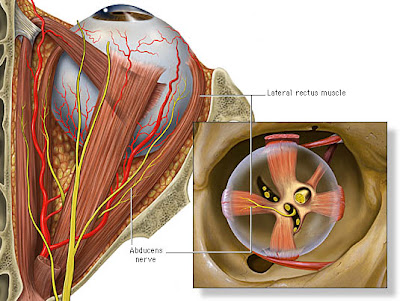
Figure 6-1a. Abducens nerve and the lateral rectus muscle.
The abducens nerve innervates the lateral rectus muscle of the ipsilateral orbit.
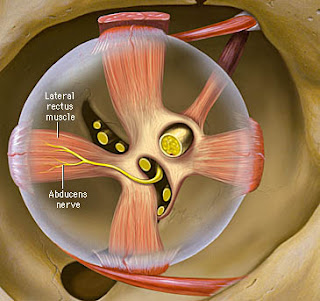
The lateral rectus muscle is responsible for lateral gaze (its contraction causes the eye to be abducted):
Figure 6-1b. Actions of the lateral rectus muscle.
Origin and central course
The fibers of the abducens nerve originate from the abducens nucleus located in the caudal pons at the level of the facial colliculus.
The nucleus is located just ventral to the fourth ventricle near the midline. Axons of CN VII (facial nerve) loop around the abducens nucleus and give rise to a bulge in the floor of the fourth ventricle - the facial colliculus.
Fibers leaving the abducens nucleus travel ventrally to exit the brainstem at the border of the pons and medullary pyramids.
Figure 6-4. Origin and central course.
Intracranial course
Upon exiting the brainstem the abducens nerve climbs superiorly along the ventral surface of the pons. On reaching the apex of the petrous portion of the temporal bone the nerve makes a sharp turn anteriorly to enter the cavernous sinus.
The abducens nerve travels along the lateral wall of the cavernous sinus with CNS III, IV, and V.
Figure 6-4. Intracranial course of abducens nerve.
Intracranial course and final innervation
From the cavernous sinus the abducens nerve enters the orbit through the superior orbital fissure.
CN VI passes through the tendinous ring of the extraocular muscles and innervates the lateral rectus muscle on its deep surface:
Figure 6-4. Final innervation of abducens nerve.
Coordination of lateral rectus and medial rectus muscles
The exact control of eye movements requires input from integration centers in the brain that coordinate the output from the occulomotor, trochlear, and abducens nuclei which control the six extraocular muscles.
For eye movements in the horizontal plane, the lateral rectus muscle of one eye and the medial rectus muscle of the other eye must work precisely together.
The actions of these muscles is coordinated by the lateral gaze center located in the pontine reticular formation.
Inputs from higher centers of the brain synapse in the lateral gaze center, which then sends simultaneous signals to the ipsilateral abducens nucleus and to the contralateral occulomotor nucleus via the medial longitudinal fasciculus.
The abducens nucleus sends signals via CN VI to the lateral rectus muscle of the ipsilateral orbit to command that eye to be abducted. Simultaneously, the occulomotor nucleus generates a command via CN III to contract the medial rectus muscle of the contralateral orbit resulting in adduction of that eye.
The end result is that both eyes precisely fixate on or track the same object.....
Clinical correlation - lower motor neuron (LMN) lesion

Damage to the abducens nucleus or its axons results in weakness or paralysis of the ipsilateral lateral rectus muscle.

This is indicated by:

Medially directed eye on the affected side due to the unopposed action of the medial rectus muscle.

Inability to abduct the affected eye beyond the midline of gaze (up to approximately the midline, the superior and inferior oblique muscles can abduct the eye).

Strabismus - the inability to direct both eyes to the same object. When asked to look at an object located laterally to the side of the lesion, the patient's affected eye will be unable to be abducted beyond the midline of gaze. The opposite normal eye will be adducted to effectively fixate on the object.

Horizontal diplopia (double vision) due to the strabismus. Patients may compensate by turning their head so that the affected eye is focused on an object and then moving the normal eye so as to fixate on the object.

CN VI paralysis is the most common isolated palsy due to the long peripheral course of the nerve.
Damage to the abducens nucleus or its axons results in weakness or paralysis of the ipsilateral lateral rectus muscle.
This is indicated by:
Medially directed eye on the affected side due to the unopposed action of the medial rectus muscle.
Inability to abduct the affected eye beyond the midline of gaze (up to approximately the midline, the superior and inferior oblique muscles can abduct the eye).
Strabismus - the inability to direct both eyes to the same object. When asked to look at an object located laterally to the side of the lesion, the patient's affected eye will be unable to be abducted beyond the midline of gaze. The opposite normal eye will be adducted to effectively fixate on the object.
Horizontal diplopia (double vision) due to the strabismus. Patients may compensate by turning their head so that the affected eye is focused on an object and then moving the normal eye so as to fixate on the object.
CN VI paralysis is the most common isolated palsy due to the long peripheral course of the nerve.
Clinical Correlation - Upper Motor Neuron Lesion

Damage to the pontine lateral gaze center may result in conjugate paralysis of lateral gaze to the affected side.

This is indicated by an inability of the patient to fixate on an object placed laterally to the affected side. Specifically it is:
Damage to the pontine lateral gaze center may result in conjugate paralysis of lateral gaze to the affected side.
This is indicated by an inability of the patient to fixate on an object placed laterally to the affected side. Specifically it is:
- Inability to abduct the eye on the affected side past approximate midline gaze. Inability to adduct the eye opposite the lesion past midline gaze.

- The end result is that neither eye is moved to effectively fixate on the target object.
| Cranial Nerve VI - Abducens Nerve | Page 8 of 8 |
Clinical correlation - MLF syndrome
Assuming the lateral gaze center is intact, damage to the medial longitudinal fasciculus (MLF) between the pons and occulomotor nucleus will result in a defect in lateral gaze.
On attempting lateral gaze:
- Due to loss of input to the occulomotor nucleus from the lateral gaze center, the adducting eye is unable to move medially past approximately the midline of gaze.

- Monocular horizontal nystagmus is observed for the abducting eye. The abducting eye moves smoothly laterally followed by a rapid movement (saccade) back to midline gaze.




No comments:
Post a Comment