6.3 Lipid Digestion, Absorption, and Transport
Lipids are large molecules and generally are not water-soluble. Like carbohydrates, lipids are broken into small components for absorption. The main goal of lipid digestion is to remove fatty acids from the glycerol backbone using the enzyme lipase. However, lipid digestion is more complicated than carbohydrate digestion because most of our digestive tract and digestive enzymes are water based. Figure 6.13 shows a general overview of what happens to lipids at each part of the digestive tract. Each step is described in more detail below.
Figure 6.13 Overview of Lipid Digestion, Absorption, and Transport
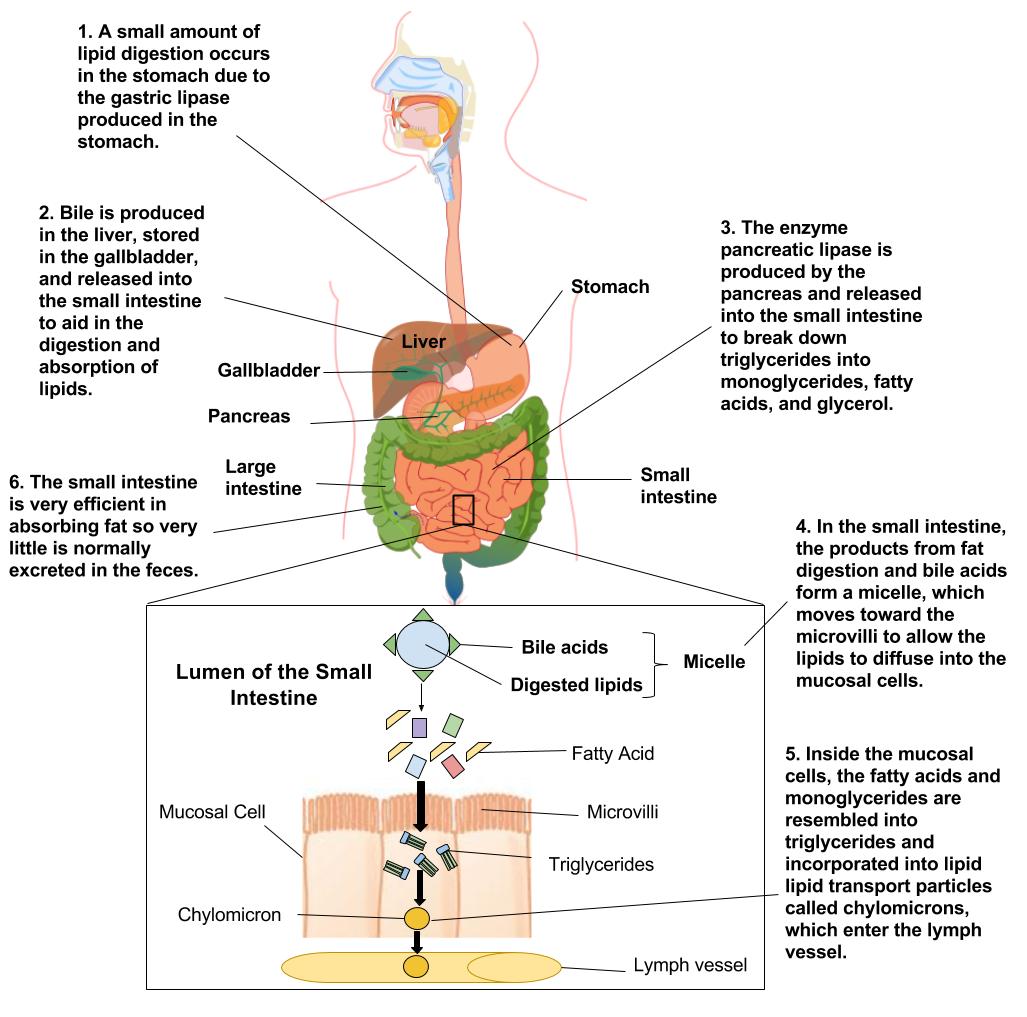
From the Mouth to the Stomach
The first step in the digestion of triglycerides and phospholipids begins in the mouth as lipids encounter saliva. Next, the physical action of chewing coupled with the action of emulsifiers enables the digestive enzymes to do their tasks. The enzyme lingual lipase, along with a small amount of phospholipid as an emulsifier, initiates the process of digestion. These actions cause the fats to become more accessible to the digestive enzymes. As a result, the fats become tiny droplets and separate from the watery components.
In the stomach, gastric lipase starts to break down triglycerides into diglycerides and fatty acids. Within two to four hours after eating a meal, roughly 30 percent of the triglycerides are converted to diglycerides and fatty acids. The stomach’s churning and contractions help to disperse the fat molecules, while the diglycerides derived in this process act as further emulsifiers. However, even amid all of this activity, very little fat digestion occurs in the stomach.
Entering the Bloodstream
As stomach contents enter the small intestine, the digestive system sets out to manage a small hurdle, namely, to combine the separated fats with its own watery fluids. The solution to this hurdle is bile. Bile contains bile salts, lecithin, and substances derived from cholesterol so it acts as an emulsifier. It attracts and holds onto fat while it is simultaneously attracted to and held on to by water. Emulsification increases the surface area of lipids over a thousand-fold, making them more accessible to the digestive enzymes.
Once the stomach contents have been emulsified, fat-breaking enzymes work on the triglycerides and diglycerides to sever fatty acids from their glycerol backbones. As pancreatic lipase enters the small intestine, it breaks down the fats into free fatty acids and monoglycerides. Yet again, another hurdle presents itself. How will the fats pass through the watery layer of mucus that coats the absorptive lining of the digestive tract? As before, the answer is bile. Bile salts envelop the fatty acids and monoglycerides to form micelles. Micelles have a fatty acid core with a water-soluble exterior. This allows efficient transportation to the intestinal cells. Here, the fat components are released and disseminated into the cells of the digestive tract lining.
Just as lipids require special handling in the digestive tract to move within a water-based environment, they require similar handling to travel in the bloodstream. Inside the intestinal cells, the monoglycerides and fatty acids reassemble themselves into triglycerides. Triglycerides, cholesterol, and phospholipids form lipoproteins when joined with a protein carrier. Lipoproteins have an inner core that is primarily made up of triglycerides and cholesterol esters (a cholesterol ester is a cholesterol linked to a fatty acid). The outer envelope is made of phospholipids interspersed with proteins and cholesterol. Together they form a chylomicron, which is a large lipoprotein that now enters the lymphatic system and will soon be released into the bloodstream. Chylomicrons transport food fats perfectly through the body’s water-based environment to specific destinations such as the liver and other body tissues.
Understanding Blood Cholesterol
You may have heard of the abbreviations LDL and HDL with respect to heart health. These abbreviations refer to low-density lipoprotein (LDL) and high-density lipoprotein (HDL), respectively. Lipoproteins are characterized by size, density, and composition. As the size of the lipoprotein increases, the density decreases. This means that HDL is smaller than LDL.
Major Lipoproteins
- Chylomicrons. These lipoproteins are made in the small intestine cells after the digestion and absorption of fat from the foods that you eat. They primarily transport exogenous, or dietary, triglycerides from the gut to the cells of the body although they also carry dietary cholesterol and fat soluble vitamins. Chylomicrons are too large to be transported in the hepatic portal vein to the liver with the water soluble nutrients. Instead they enter the lymphatic system and are deposited directly into the bloodstream via the subclavian vein. They circulate throughout the body, delivering triglycerides to the body’s cells, especially adipose and muscle tissue, where the triglyceride can be used for energy or stored for later use. The remaining part of the chylomicron, or remnant, is delivered back to the liver for disposal.
- Very low density lipoproteins (VLDLs). Very low-density lipoproteins are made in the liver from remnants of chylomicrons and transport endogenous triglycerides from the liver to various tissues in the body. As the VLDLs travel through the circulatory system, the lipoprotein lipase strips the VLDL of triglycerides. As triglyceride removal persists, the VLDLs becomes smaller and more dense.
- Low density lipoproteins (LDLs). The remnants of VLDLs are converted to LDLs. LDLs are commonly known as the “bad cholesterol” and it is imperative that we understand their function in the body so as to make healthy dietary and lifestyle choices. LDLs carry cholesterol and other lipids from the liver to tissues throughout the body. LDLs are comprised of very small amounts of triglycerides, and house over 50 percent cholesterol and cholesterol esters. How does the body receive the lipids contained therein? As the LDLs deliver cholesterol and other lipids to the cells, each cell’s surface has receptor systems specifically designed to bind with LDLs. Circulating LDLs in the bloodstream bind to these LDL receptors and are consumed. Once inside the cell, the LDL is taken apart and its cholesterol is released. In liver cells these receptor systems aid in controlling blood cholesterol levels as they bind the LDLs. A deficiency of these LDL binding mechanisms will leave a high quantity of cholesterol traveling in the bloodstream, which can build up in the arteries as oxidized plaques and lead to heart disease or atherosclerosis. Diets rich in saturated fats will inhibit the LDL receptors which are critical for regulating cholesterol levels.
- High density lipoproteins (HDLs). High-density lipoproteins are responsible for carrying cholesterol out of the bloodstream and into the liver, where it is either reused or removed from the body with bile. This is also known as reverse cholesterol transport. HDLs have a very large protein composition coupled with low cholesterol content (20 to 30 percent) compared to the other lipoproteins. Hence, these high-density lipoproteins are commonly called “good cholesterol.”
Blood Cholesterol Recommendations
For healthy total blood cholesterol, the desired range you would want to maintain is under 200 mg/dL. More specifically, when looking at individual lipid profiles, a low amount of LDL and a high amount of HDL prevents excess buildup of cholesterol in the arteries and wards off potential health hazards. An LDL level of less than 100 milligrams per deciliter is ideal while an LDL level above 160 mg/dL would be considered high. In contrast, a low value of HDL is a telltale sign that a person is living with major risks for disease. Values of less than 40 mg/dL for men and 50 mg/dL for women mark a risk factor for developing heart disease. In short, elevated LDL blood lipid profiles indicate an increased risk of heart attack, while elevated HDL blood lipid profiles indicate a reduced risk.
Current guidelines recommend testing for anyone over age twenty. If there is a family history of high cholesterol, your healthcare provider may suggest a test sooner than this. Testing calls for a blood sample to be drawn after nine to twelve hours of fasting for an accurate reading. (By this time, most of the fats ingested from the previous meal have circulated through the body and the concentration of lipoproteins in the blood will be stabilized.)
According to the National Institutes of Health (NIH), the following total cholesterol values are used to target treatment:
- Desirable: Less than 200 mg/dL
- Borderline high: 200–240 mg/dL
- High risk: Greater than 240 mg/dL
According to the NIH, the following desired values are used to measure an overall lipid profile:
- LDL: Less than 160 mg/dL (if you have heart disease or diabetes, less than 100 mg/dL)
- HDL: Greater than 40–60 mg/dL
- Triglycerides: 10–150 mg/dL
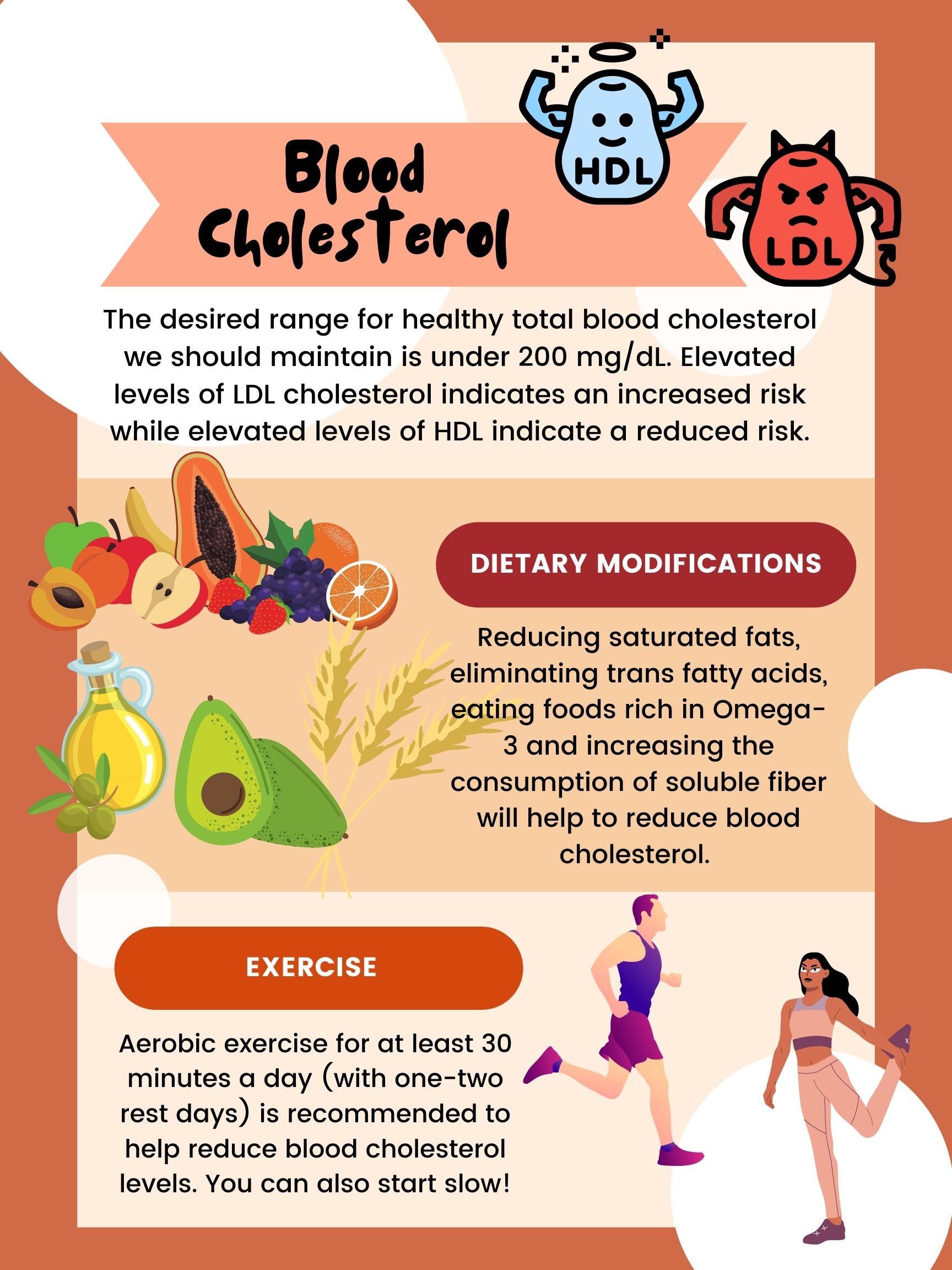
If your blood cholesterol numbers are not ideal, Figure 6.14 provides some lifestyle modifications that can help improve your cholesterol. For some people, especially if you have a family history of high cholesterol, medication will be required. Please consult with your doctor.
Figure 6.14 Improving Your Blood Cholesterol
Media Attributions
- Lipid Digestion and Absorption © Allison Calabrese is licensed under a CC BY (Attribution) license
- Blood Cholesterol © Natalie Fox is licensed under a CC BY (Attribution) license
