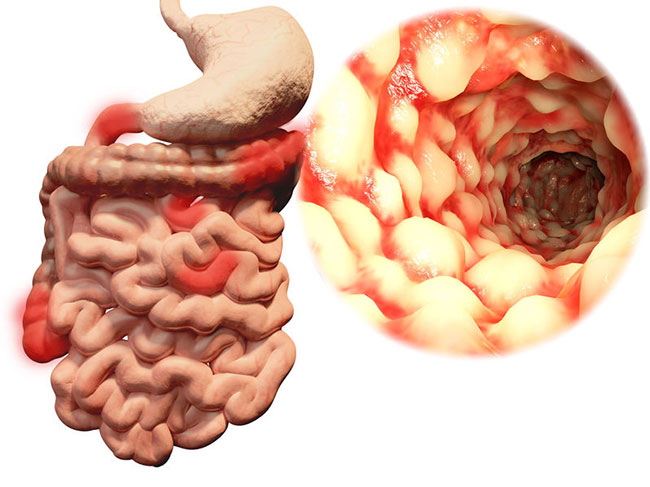
In this article I am going to discuss the role of inflammation in the gut with a particular focus on Crohn’s disease. We’ll look at the main symptoms, probable causes and what you can do to help improve your outcome.
What is Crohn’s Disease?
Crohn’s disease is one of the illness’s that comes under the umbrella term of Inflammatory Bowel Disease (IBD). Each is different, but all involve significant inflammation in the gut.
Crohn’s can occur anywhere along the digestive tract, but it is commonly found in the colon or lower parts of the small intestine.
In many cases inflammatory reactions are noted throughout the bowel wall, however in some people the inflammatory lesions can be non-existent or somewhere in between making diagnosis more challenging and less obvious.
Symptoms of Crohn’s
The most common symptoms in Crohn’s disease include abdominal pain and discomfort, loose stools and increased frequency, weight loss or struggling to gain any weight and potentially malnutrition as well. Some people experience significant loss of appetite and low-grade fever.
Because of it’s impact on digestion and absorption of nutrients it has the potential to cause all sorts of symptoms, especially when not well managed. People will often notice poor hair, skin and nail health and things like significant fatigue as their symptoms worsen.
Diagnosis of Crohn’s
Diagnosis should come from a medical professional such as a qualified gastroenterologist. Combinations of different tests are usually required such as colonoscopy (camera up the backside), where they may also take tissue samples. Sometimes they may do a wireless capsule that will take images along the way once swallowed.
Blood tests to look at inflammatory markers and also for signs of anemia/malnutrition along with signs of infection can also be used to look for signs of Crohn’s.
Stool samples looking at inflammatory markers such as calprotectin and lactoferrin may also be useful to differentiate between IBS diagnosis and IBD.
There are also certain specialist scans used to examine the small intestine as well.
If in doubt speak to your GP and look at getting a referral to a gastroenterologist who will be able to help you further.
The stool testing that I use will assess calprotectin and utilising that alongside symptoms, health history and perhaps indications on one’s blood test can give me good reason to suspect IBD and refer out for diagnosis while we work on underlying causes of your digestive health issues.
What causes Crohn’s disease?
Here goes the million-dollar question. When it comes to health there is rarely a single factor that leads to a single condition, in fact if things where that simple in health, getting fixed would be pretty easy.
There are a number of potential contributing factors that I will discuss now.
Blaming genes?
Genetics seem to play a considerable role in the development of Crohn’s. In fact nearly all cases that I have seen the individuals have close family members that have been diagnosed with the same or similar conditions.
However, gene’s should never be blamed for everything, there also has to be environmental triggers that result in the development of immune & inflammatory imbalances that lead to conditions like Crohn’s. Below I discuss some of those contributing environmental factors.
Imbalances in bacteria
The evidence is clear that imbalances in bacteria in the intestine can play a role in the development of Crohn’s.
One of the amazing jobs our bugs do in our gut is play a crucial role in immune modulation, helping to keep our immune system balanced and inflammation under control. This is in part achieved through their protective effect on our intestinal wall.
The 100 trillion+ bugs we find in our gut when balanced help to keep bad bugs under control, support nutrient absorption and synthesis and prevent our digestive lining from becoming damaged and leaky. 99.99% of the time it is the job of the immune system to not respond, however when the gut barrier becomes compromised in a process known as intestinal hyperpermiability or “leaky gut” the immune system starts responding to things it perhaps would not have done so before such as some of the foods that you are eating.
Increases in certain bacteria such as bateroides and lower levels of bifidobacter species seem to be associated with the development of Crohn’s disease.
E.Coli is also linked with Crohn’s, along with staphylococcus, streptococcus, proteus disease, mycoplasma pneunoniae, clostridium Difficile, chlamydia psittaci.
Bacterial infections appear in ¼ of all recurrent cases so it is worth running a comprehensive stool analysis which looks at a variety of pathogenic bugs, opportunistic bugs and your normal bacteria flora like your bifidobacter species.
Poor dental hygiene has also been linked with the development or increased risk of IBD, and past cases of food poisoning increases risk as well for their disturbing effect on the microbiome.
Antibiotic exposure
Heavy use of antibiotics since the 1950’s has been linked with an explosion in the occurrence of Crohn’s, posing the question whether antibiotics are to blame in this epidemic. It is unlikely they are the sole underlying cause but in genetically susceptible individuals and in combination with certain nutrition, lifestyle and environment factors it appears to increase risk.
Other medications seem to be linked as well including the use of non steroidal anti-inflammatory drugs such as ibuprofen and a drug I have seen a lot in people I consult with called Accutane (isotretinoin), something commonly used alongside lengthily antibiotic courses in the treatment of acne. Read more about some ideas on natural approaches to dealing with acne.
Infections & Immune Imbalances
In a number of cases the development of Crohn’s follows an infection of some kind, whether bacterial, parasitic or viral. It is sometimes worth looking at your health timeline to determine if an infection may well have triggered off the onset of your symptoms.
Some people appear to have seasonal flare ups, suggesting an immune/allergy component to the disease, so it is worth noting if symptoms flare at certain times of the year and then looking at food and environment exposures at that time.
Nutrition
This is where it gets interesting. Nutrition is rarely considered, however what we eat has been linked with Crohn’s and actually plays a crucial role in the development but also the management of Crohn’s as well.
Food plays a crucial role in the development of a healthy digestive system and an imbalanced diet can lead to imbalances in the bacteria present in the gut. Significant changes in our microbiome from the food we eat can take as little as 2 days.
A general increase in a more pro-inflammatory diet such as the British Average Diet (BAD) or Standard American Diet (SAD) appears to be linked with increased occurrence of Crohn’s. Higher intakes of omega-6 fats, in particular more processed vegetable oils, high grain and sugar intake and lower fruits and veg intake, thus less prebiotic foods seem to be linked.
Over consumption of high fat meats also appears to be linked and can drive inflammation further, particularly low-grade and processed meats and dairy.
There is also a drop in our natural intake of omega-3 fatty acids, in particular those found in oily fish. Add to that intensive farming of these fish, which can impact the omega 3/6 ratio. You may have noticed how much fattier farmed fish is over wild fish, in fact it has around twice as much fat, and unfortunately that does not equate to twice as much omega-3 fatty acids. Saturates increase 3 fold and omega 6 fatty acids around 5 fold in farmed salmon as an example.
Natural considerations to help Crohn’s
Change your diet
As with all digestive health complaints a change in diet is often useful to help control symptoms but also to help address underlying issues as well as just supporting general health. There is literally nothing to lose and plenty to gain by adopting a healthier diet.
As mentioned earlier inflammation can be driven by certain dietary factors, so here is a quick guide to some nutrition changes you may want to make:
- Reduce intake of omega-6 fats and emphasize natural sources of omega 3 like wild oily fish.
- Avoid a highly saturated fat diet, especially of poor protein sources like conventionally grain fed meats and dairy or processed meats and dairy.
- Choose leaner proteins, and Mediterranean oils like olive and avocado.
- Eat a variety of fruits and veg and test out levels of fiber and prebiotics in your diet. Sometimes a high fiber diet helps and other times it can hinder, so increase your fiber intake slowly but surely to avoid unpleasant side effects. Typically I have found fiber from fruit and veg seems to help whereas high fiber grain foods appear to challenge the body and can exacerbate symptoms with some exceptions like well soaked oats. Often a modified elimination diet where you go grain free in the initial stages can be very useful.
- Initial elimination of gluten, dairy, and carrageenan-containing foods. Carrageenan is used commonly for it’s thickening and stabilizing properties so check your labels.
Consider adopting an elimination diet. I have written some basics on the Elimination diet to help you understand more about that process. This is something I strongly recommend you have professional support with, as it is not something that is right for everyone, especially those with past issues with food or those in an already emaciated state. It needs to be well planned and have ongoing support from a professional. To help my clients I have created many documents containing food lists, recipes, meal planners etc.
Short-term use of an elemental diet may also help reduce symptoms and reset the immune system, again this requires professional support as it is much more of an acute therapeutic tool and not a long term adaptation.
Another diet that seems to help is the specific carbohydrate diet (SCD). Elaine Gottschall’s book breaking the vicious cycle may help with this and again this is another approach.
Pre & Probiotics
Various studies have demonstrated a benefit when using probiotics to help with IBD, but it tends to be a little more associated with Ulcerative Colitis.
Probiotic supplements can have a temporary impact on the balance of bacteria in the gut, this can often help acutely, however they do little to help the long-term environment. For that reason I would recommend prebiotic and probiotic foods long term and only acute use of probiotic supplementation.
Prebiotic foods help to feed the good guys in our digestive system and any diet, no matter what your health issue, should contain good levels of these foods.
You can also use probiotic foods, something has been out of fashion for some time but we are seeing more of now.
Check out my article on pro and prebiotic foods.
The bacteria in our gut can be useful in stimulating our immune response by increasing antibodies such as SIgA, IgM and IgG and support the integrity of the gut lining, helping to prevent leaky gut I was speaking about earlier so they should not be underestimated.
Anti-inflammatories and immune modulators
Many conventional treatments focus on trying to lower inflammatory responses, thus it would make sense to use some natural therapies that are able to offer a similar support such as fish oil and curcumin from turmeric. Fish oil also has immune suppressing effects as well as inflammation suppressing effects, which can be useful in cases of IBD, especially in the acute phases but also at lower dosages for maintenance.
Natural COX2 inhibitors such as green tea, boswellia and again curcumin may be of use.
Foods sensitivity testing
Testing the foods we eat for immune responses can be useful especially when there are few signs of infection in the bowel or an elimination diet is not suitable for that individual. I have seen excellent improvements with Crohn’s symptoms when eliminating foods that appear to challenge the immune system through non-allergy pathways such as the IgG immune pathways. Using these tests and designing a diet based around the correct foods, I have seen a significant reduction in the frequency of bowel movements. In one case we managed to reduce one of my clients bowel movements from around 10-15 x per day to around 3 x per day by adapting his diet off the back of IgG testing.
There are limitations with IgG testing and no real standardisation of testing. This makes it a controversial test to use even though there is emerging evidence of IgG testing being useful with IBS and migraines. My view is that it can be useful in some cases however where possible I will utilise the gold standard elimination diet instead.
Nutritional Support through supplementation
Because Crohn’s can significantly limit absorption capabilities if may be worth looking into some additional nutrient support. This can be delivered using pills, powders, sublingual’s and topical delivery methods. In some rare more severe cases IV nutrient therapy and intramuscular injections may be useful to completely bypass the gut and deliver higher dosages.
Zinc, B12 and folate are common deficiencies in Crohn’s patients, thus regular blood work is important and supplementation may be required. I’d usually recommend sub lingual in the case of B12 and folate in Crohn’s patients showing signs of deficiency.
Electrolytes and trace mineral support are often crucial in those suffering with frequent loose stools and can be added to water consumed in the day. Its worth getting a good electrolyte supplement as many are also loaded with sugar which can exacerbate imbalances of bacteria in the gut.
It may also be worth looking at the potentially depleting effect some medications can have on specific nutrients in the body and replace or support where required so long as there are no negative interactions between the supplement and medication. A nutritional professional will be able to assess whether any medications you are on can have depleting effects on certain nutrients and whether certain nutrients are contraindicated with the medications you are taking.
Because Crohn’s has a significant immune component, ensuring good levels of vitamin D can be important as vitamin D helps to modulate the immune system. Low vitamin D may be due to poor absorption, although mostly metabolised from sun exposure, you can easily use cream and sublingual forms to bypass the gut and optimise Vitamin D.
Vitamin A is another fat soluble vitamin like Vitamin D. Interestingly Vitamin A is crucial for the integrity of your intestinal lining and low levels may exacerbate leaky gut.
Glutamine is an amino acid. Generally it is quite abundant, however the intestinal tract is the greatest user of glutamine as the cells that make up our gut wall use them as their principle fuel.
A more recent compound to help with different forms of IBD includes serum derived immunoglobulin proteins and early research looks promising.
A slightly more leftfield approach has been the recent use of other worms/parasites known as helminthes like Trichuris suis or Necator americanus to help modulate an imbalanced immune system helping to address IBD.
Helping to sooth symptoms can also be useful, so the use of demulcents such as slippery elm, marshmallow root and Deglycyrrhizinated licorice/DGL can be useful.
Reduce Stress
Emotional support is important. Stress can act as a trigger to any gut/immune imbalance. Likewise a diagnosis and the stress that surrounds food and your symptoms can also be quite challenging.
Often when diagnosed with a condition we tend to own that condition and we look for symptoms associated with it. Having a positive mindset and viewing your challenges differently is important in the long-term management of Crohn’s disease.
We should not search for symptoms, instead be pleasantly surprised if they are not there.
Mindfulness based stress reduction techniques are useful and activities such as yoga, meditation, Thai Chi, Qi Gong, Heart Rate Variability training and basic diaphragmatic breathing should be seen as useful tools in the recovery and management of Crohn’s.
Fecal matter transplants
This might sound gross and that is because it is, but an increasing area of research with significant cases of Crohn’s is the use of Fecal Matter Transplant (FMT). FMT is when you take the feces from a healthy individual and insert it into the bowels of someone with Crohn’s.
As with the infection Clostridium Difficile, it is also showing promise in inflammatory bowel disease conditions like Crohn’s. It’s early days in the research in this area, but watch this space as future treatment of Crohn’s might involve you swallowing someone else’s feces, nice!
Primary Nutrition Intervention
Adopting some type of hypoallergenic elimination or elemental diet should be a good starting point. Slow introduction of prebiotic foods and possibly probiotic foods may be useful as well.
Primary Supplements
- Fish Oil
- Turmeric (curcumin) and Boswellia
- Wormwood
- Glutamine
- Vitamin D – Check Bloods First
Secondary Supplements
- Multinutrient formula – good levels of B12/folate and zinc
- Aloe vera and glutamine combinations
- Possibly prebiotics
- Possibly probiotics – bifidobacter species and the competitive yeast saccharomyces Boulardii
- Helminths Therapy
- Consider adding collagen supplements to shakes or drinks or better yet making your own bone broth would be a good idea
- Demulcents such as slippery elm, marshmallow root and deglycyrrhizinated licorice/DGL
Testing Considerations
- Stool testing for underlying infection or bacterial/yeast imbalances
- Leaky gut
- Immune based food sensitivity testing
- Comprehensive Blood Chemistry with nutrient analysis such as Vitamin D, Vitamin A, Zinc, B12, folate, Omega 3 to 6 ratio
Lifestyle Considerations
- Reduce stressors and work on stress reduction/reframing
- Eliminate smoking
I hope this review helps provide some direction and perhaps hope that natural therapies can play a role in the management of IBD and specifically in Crohn’s disease.
If you would like nutrition and lifestyle support with the management of Crohn’s, other IBD or general digestive health symptoms please fill out the contact form at the bottom of this page to enquire about 1-2-1 consultation services.
[widgetkit id=”407″]
Contact Steve Grant Health
To learn more out how Steve Grant Health can assist you on your journey, please fill out the enquiry form below.
Please note that depending on your specific circumstances and goals, Steve may recommend that you work with one of the specialist practitioners within his network of trusted professionals.
If you have been referred by a clinician, please complete the form and ensure that you state who has referred you or have your practitioner email Steve direct to make a referral that way.
Click the button below to open the client enquiry form:
[widgetkit id=”643″]