Orthodontic appliances for patients with a nickel allergy
Published: 01/09/2013
Nickel is the metal most likely to cause an allergic reaction and is also present in many orthodontic appliances. This article examines what a nickel allergy is and the considerations involved for patients with the condition
An allergy to nickel is one of the most common causes of allergic contact dermatitis— an itchy rash that appears when a normally harmless substance touches the soft tissue. Nickel is one of the metals most commonly found in materials that are used to make orthodontic appliance components, with the element being present in stainless steel, nickel–titanium and other alloys.
A significant increase in the level of nickel in saliva and serum has been found in patients following the insertion of fixed orthodontic appliances. Nickel is also the metal that is most likely to cause contact dermatitis in patients with orthodontic appliances. The first part of the article will look at the causes, signs, symptoms and epidemiology of a nickel allergy, and ways in which the reaction is diagnosed will be explained. The article will go on to focus on the nickel content of orthodontic appliance components and examine the alternative products that are either nickel-free or have a very low nickel content that are suitable for patients with the allergy.
History and etymology
When a red mineral that resembled copper-ore was found in the medieval German Erzgebirge (Ore Mountains), miners who were looking for copper could not extract any copper from it. The ore they extracted was found not to contain any copper and it also made them ill. A mischievous sprite of German mythology, Nickel (similar to Old Nick), was blamed for besetting the copper (German: Kupfer) and it became known as kupfernickel (copper of the devil or ‘false copper’). This German equivalent of ‘copper-nickel’ was used as early as 1694. Kupfernickel was also known as rotnickelkies and arsennickel in old German. In modern German, kupfernickel and kupfer-nickel designates the alloy cupronickel. Nickel was first isolated and classified as a chemical element in 1751 by Swedish mineralogist and chemist Baron Axel Fredrik Cronstedt when he was working as a mining expert with the Bureau of Mines Copper. While attempting to extract copper from Kupfernickel, he discovered a silvery metal that he named after the sprite, nickel.
Aetiology
A nickel allergy occurs because the immune system has an excessive reaction to the material. The immune system reacts to protect the body against bacteria and viruses. Once the body has developed a reaction to a particular agent (allergen), the immune system will always be sensitive to it. An allergic response can be described as a response where certain parts of the immune system have an excessive reaction to a foreign material. Nickel can bring out contact dermatitis (Figure 1), which is a Type IV delayed hypersensitivity immune response (van Loon et al, 1988; Aaolu et al, 2001). This involves two interrelated, distinct phases; first, a phase of sensitisation occurs as soon as the allergen enters the body, is recognised and a response takes place. This is followed by the elicitation phase, which transpires after re-exposure to the allergen to the appearance of the full clinical reaction. It is possible that no symptoms were present during the initial exposure to the material, but successive exposure then leads to a more visible response.

Figure 1.Contact dermatitis
In those patients who are predisposed, nickel is the most common metal causing allergy (Kalimo et al, 2004; Saglam et al, 2004; Schultz et al, 2004) but, as yet, there is no evidence of its direct toxicity (David and Lobner, 2004; Eliades et al, 2004).
Signs and symptoms of nickel allergy
Extraoral symptoms of a nickel allergy include urticaria (hives), a flare-up of allergic dermatitis, eczema or an exacerbation of any pre-existing eczema. Intraorally, patients with a nickel allergy can present with stomatitis (inflammation of the oral mucosa) from mild to severe erythema (reddening), papula peri-oral rash, a metallic taste or a loss of taste, soreness at side of the tongue, numbness, burning sensations, angular cheilitis (inflammation of the lip), and severe gingivitis in the absence of plaque.
Diagnosis
If a patient presents with any of the above signs and symptoms after they have been fitted with an orthodontic appliance, and has had previous allergic responses from metallic jewellery, watches, belt buckles or studs, they are likely to have a nickel allergy. The diagnosis should be confirmed by a dermatologist who would carry out a patch test.
Epidemiology
It is estimated that 4.5–28.5% of the total population are sensitised to nickel (Peltonen, 1979). Peltonen reported that nickel hypersensitivity was more prevalent in females than in males by 10 to 1. This disproportionate hypersensitivity in females was thought to be because of their more frequent contact with jewellery, such as earrings (Figure 2). This gender bias has also been reported in a later study by Kerosuo et al (1996). This study looked at 700 Finnish adolescents aged 14–18 years, and found that 68% had worn orthodontic appliances containing nickel. Females were found to be significantly more disposed to nickel allergy, with 30% of the girls and only 3% of the boys affected.

Figure 2.A stud earring
The piercing of ears also had a significant affect. In the 1996 Finnish study, 31% of subjects with pierced ears were shown to have nickel hypersensitivity, while only 2% of those without pierced ears were found to have the allergy. Whether the subjects had worn orthodontic appliances did not seem to affect the prevalence of nickel hypersensitivity; the results even suggested that treatment with orthodontic appliances containing nickel before ear piercing may have reduced the occurrence of nickel hypersensitivity—as none of the girls who were treated with fixed orthodontic appliances before piercing had nickel hypersensitivity but 35% of the girls who had had their ears pierced before the onset of orthodontic treatment were sensitised to nickel.
Orthodontic appliance considerations
Orthodontic appliances that contain metal can cause allergic reactions due to the release of metal ions, such as nickel, into the mouth. Bass et al reported concerns about sensitising patients to nickel through routine treatment with fixed orthodontic appliances in 1993. Once a patient has become hypersensitive to nickel it can affect all the oral mucosal tissues.
Jia et al (1999) found that these ions are released due to many factors, including composition of the metal, abrasion, friction wear due to sliding mechanics, strain of the wire, presence of solder, pH and temperature of the environment. The two most popular metals used in orthodontics containing nickel are stainless steel (up to 9% nickel) and nickel–titanium (up to 50% nickel). Through research of current orthodontic material manufacturers and suppliers, all commonly used appliance components can be replaced with a titanium or low nickel content stainless steel alternative (Green, 2010). Table 1 gives examples of the nickel-free and low-nickel products that are currently available.
Table 1.
Examples of nickel-free and low-nickel products that are currently available
Nickel–titanium
Nickel–titanium alloys contain nickel and titanium in approximately equal measure; wires with this level of nickel content are thought to bring on nickel hypersensitivity (Jia et al, 1999) and should be avoided for nickel-sensitive patients. Many archwires for fixed orthodontic appliances are made from nickel-titanium but alternative wires made from 100% titanium or titanium– molybdenum alloy (TMA) are available. Resin- or plastic-coated nickel–titanium archwires would also be suitable for these patients too (Kim and Johnson, 1999).
Stainless steel
Stainless steel is a generic term for a family of corrosion-resistant alloys containing 10.5% or more chromium. Spring hard stainless steel (EN-standard Steel no: 1.4310) used in orthodontics contains up to 9% nickel (Figure 3). Most studies have concluded that patients with a nickel allergy are able to wear appliances with stainless steel elements without a noticeable effect. This is thought to be because of the crystal lattice structure of the alloys binding the nickel, meaning that the offending metal is not free to react (Toms, 1988). People who have reported nickel hypersensitivity due to stainless steel wire either used the wire for intermaxillary or internal fixation following orthognathic surgery, were not tested for corrosion or had a higher nickel content (Shriver et al, 1976; Guyuron and Lasa, 1992).
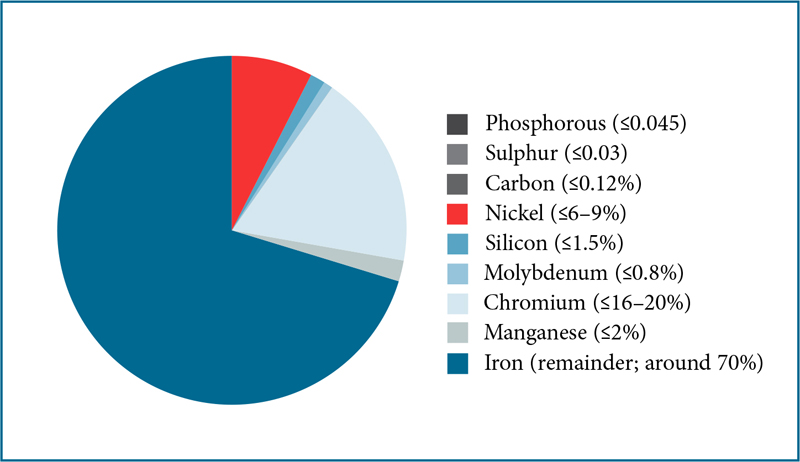
Figure 3.Typical composition of stainless steel
Stainless steel has many applications in orthodontics, and different gauge wires are used to fabricate different elements. A type of stainless steel with a low nickel content (EN-standard Steel no: 1.4456) is available in all the necessary wire gauges and only contains a trace amount of nickel (= 0.2%;
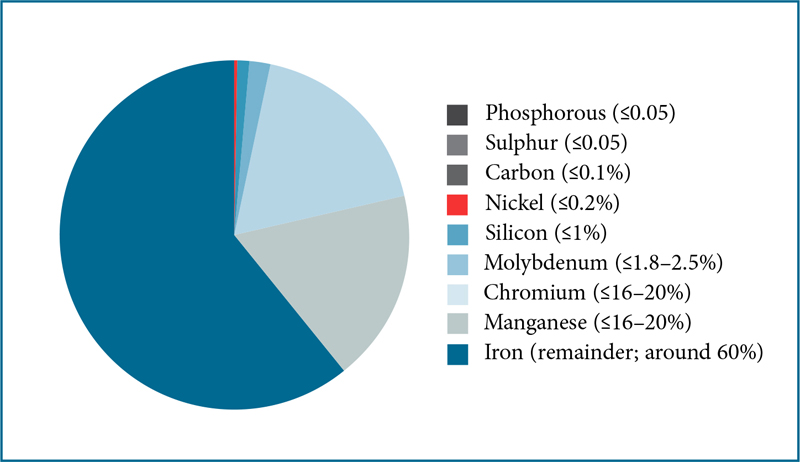
Figure 4.Typical composition of low nickel stainless steel

Figure 5.Low-nickel stainless steel wire from Forestadent
Orthodontic brackets are also usually made from stainless steel but there are alternatives available made from either low-nickel-content stainless steel titanium, polycarbonate or a ceramic material (made using polycrystalline alumina, single-crystal sapphire, and zirconia). Another use of stainless steel in orthodontics is for the manufacture of preformed ball clasps, which are a popular fixation component for removable appliances, and are often used for anterior retention of lower twin-block appliances. Low-nickel stainless steel ball clasps are also available (

Figure 6.Low-nickel stainless steel ball clasps from Dentaurum
Other stainless steel orthodontic appliance components, such as multistrand wire, commonly used for fixed retainers, expansion screws and rapid maxillary expansion screws, can be replaced with titanium alternatives. Titanium is widely considered to be the most biocompatible of all metals because of its ability to remain inert in the body, withstand attack from bodily fluids and stay compatible with bone growth. Titanium multi-strand wire is available from Dentaurum (

Figure 7.Titanium triple-strand retainer wire from Dentaurum

Figure 8.Titanium expansion screws from Dentaurum
Conclusion
While severe allergic reactions to nickel in patients with orthodontic appliances may be rare, it is good practice for all dental professionals to be aware of the risks attached to certain orthodontic materials, and to avoid their use in susceptible patients, especially as more suitable alternatives are readily available.
position="float" orientation="portrait">KEY POINTS
Nickel is the metal most likely to cause an allergy and is present in many orthodontic appliances.
Orthodontic appliances can cause a patient to develop a nickel allergy, especially appliances containing nickel–titanium.
Materials that contain a high quantity of nickel should be avoided for patients with a nickel allergy.
All commonly used orthodontic appliance components can be replaced with a titanium or low-nickel-content stainless steel alternative.
Author: MA Healthcare
Please sign in or subscribe to continue reading.
The following article is restricted for Dental Nursing subscribers only. Please sign in to access the full article.
If you have any queries or require more information, Dental Nursing’s friendly customer services team is on hand to help. Call 01722 716997 or email subscriptions@markallengroup.com.
Subscribe to Dental Nursing below and get access to this article. Subscribing will enable you to:
- Update your knowledge in important areas of practice.
- Keep fully up-to-date with the latest developments taking place in clinical practice as they affect you.
- Access restricted content and our CPD platform.








.jpg?width=150&height=100&scale=canvas)




