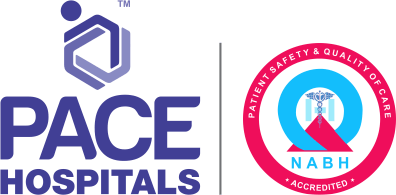
Crohn's Disease - Symptoms, Types, Causes, Complications & Prevention
Crohn’s disease meaning
Crohn's disease is an immunologically mediated chronic inflammatory bowel disease (autoimmune disorder) of the gastrointestinal (GI) tract that extends along the whole gut wall thickness, from the mucosa (inner layer) to the serosa (outer layer). Crohn's disease can advance from mild /moderate inflammatory conditions to severe piercing (fistulisation) or structuring illness with multiple relapses.
In Crohn's disease, the immune system targets the gut, resulting in bowel inflammation, leading to a bowel blockage, severe diarrhoea, painful bowel movements, rectal bleeding, and other severe symptoms through destruction of the intestinal tissue.
The disease has recurrent and remitting symptoms such as severe diarrhoea, weight loss, malnutrition, and abdominal pain. Nearly one-third of patients have small bowel involvement, particularly in the terminal ileum; 20% have only colon involvement, and 50% have both the colon and small bowel involved.
The Crohn’s disease cure is still under research, as there is no permanent treatment for this condition, and the majority of patients go through unexpected remission and relapse cycles. The average Crohn’s disease life expectancy will be shorter compared to those without the illness.
Juvenile Crohn’s disease
Juvenile Crohn's disease is also termed paediatric Crohn's disease, a rare form of inflammatory bowel disease characterised by chronic inflammation of the intestinal wall or any part of the GI tract. Poor linear growth and insufficient weight gain are frequently presenting problems in children. Although adults are more likely to be diagnosed with Crohn's disease, adolescents and teenagers make up about 25% of all diagnoses that just affect the small intestine.
Types of Crohn's disease
Based on the inflammation location in the gastrointestinal tract (GI), they are classified as follows:
- Ileocolitis
- Ileitis
- Gastroduodenal Crohn’s
- Jejunoileitis
- Crohn's (granulomatous) colitis
- Ileocolitis: The most typical form of Crohn's disease that causes inflammation of the colon (large intestine) and the terminal (last) part of the ileum (small intestine)
- Ileitis: Inflammation in the terminal ileum
- Gastroduodenal Crohn’s: Inflammation of the stomach and duodenum (initial part of the small intestine)
- Jejunoileitis: Inflammation of the jejunum, a middle part of the small intestine
- Crohn's (granulomatous) colitis: Inflammation of the colon
Incidence and prevalence of Crohn’s disease in India
As per 2012-2013 data, the mean annual incidence was reported as 3.91 (3.31-4.57) per 1,00,000 people, which is more than the pooled data of Southeast Asia (0.36; 0.28-0.46) and East Asia (0.34; 0.17-0.68). Read the report
The rising frequency of Crohn’s disease in India may be related to the combination of dietary, genetic and environmental factors. Overall, the incidence and prevalence of Crohn’s disease in the Asia-Pacific area are reported to be lower than those in North America or Europe. Read the report
Crohn's disease causes
Crohn's disease, a category of inflammatory bowel disease (IBD), has a complex genetic and environmental basis, but its precise cause is still idiopathic (unknown). The disease appears to be caused by an inappropriate intestine's immune system to medications, toxins, infections, or intestinal bacteria in a genetically susceptible host. However, the likelihood of having the disorder may be higher with the following risk factors:
- Autoimmune disease
- Smoking
- Genes
Over a hundred genes connected to IBD have been found with a genetic link with Crohn's disease, particularly the NOD2/CARD15 mutations. These mutations are associated with ileal (last part of the small intestine) involvement, greater severity of ileal illness necessitating surgical intervention / reoperation, and diagnosis at a younger age.
Crohn’s disease symptoms
Crohn's disease symptoms can vary in males and females from minor to severe and develop gradually. Any area of the small or large intestine may be affected by Crohn's disease (intestinal symptoms). In addition, it also manifests with extraintestinal symptoms.
Intestinal symptoms of Crohn's disease
- Difficult to pass stools
- Pain and cramps in the abdomen
- Feeling of an incomplete bowel evacuation
- Bleeding in the rectum
- Urgency is passing bowel
- Persistent diarrhoea
- Anal fistulas/Anal fissures
Extraintestinal manifestations (symptoms) of Crohn's disease
Systemic symptoms outside the GI tract caused by inflammatory bowel disease (IBD) can significantly impact a patient's health and quality of life.
- Increase in body temperature.
- Sweating during nights
- Stones in kidneys
- Osteoporosis (decrease in bone mineral density and bone mass)
- Reduction in weight
- General malaise
- Back pain
- Abnormal menstrual cycle
- Sores in mouth
- Joint pains
- Skin rashes
- Loss of hunger
- Vision problems
Crohn’s disease symptoms in females
Most females with Crohn's disease begin to exhibit symptoms before the age of 35. Women may experience certain specific symptoms, such as:
- Oligomenorrhea (Irregular periods)
- Dyspareunia (pain in genitals before/during/after intercourse)
- Deficiency in iron
- Low fertility
Crohn’s disease complications
Crohn's disease has both intestinal (local) and extraintestinal complications (systemic). The following are a few of them.
Intestinal (local) complications include
- Stricture formation (swelling and scarring of intestinal walls)
- Malabsorption and malnutrition.
- Fistulae and abscesses
Extraintestinal (systemic) complications include
- Arthritis - Ankylosing spondylitis
- Skin problems - Pyoderma gangrenosum (painful sores on the skin), Skin tags, Erythema nodosum (painful bumps under the skin)
- Eye problem (Crohn’s disease eyes) - Scleritis (inflammation of the sclera), Uveitis (inflammation of the eye), Episcleritis (inflammation of episcleral)
- Renal problem - Hydronephrosis (swollen kidneys build-up of urine), Kidney stones
- Liver and pancreatic problems - Gall stones, Fatty liver disease, Pancreatitis (inflammation of the pancreas), Hepatitis (inflammation of the liver)
- Anaemia (reduced count of red blood cells)
- Colorectal cancer
- Mouth ulcers
- Osteoporosis (reduced bone mass and mineral density)
Crohn’s disease risk factors
The following are the Crohn's disease risk factors that increase the chance of having the disease, that include:
- Age (< 30 years)
- Smoking
- Usage of anti-inflammatory medications
- Family history of Crohn’s disease
- Increased consumption of high-fat or processed foods
- Presence of bacterial infection
Crohn's Disease Prevention
Crohn’s disease cannot be prevented; however, the following might lessen flare-ups and ease symptoms:
- Quit smoking
- Daily yoga for stress management
- Avoid intake of painkillers
- Consumption of a low-fat diet
- Regular exercise
Crohn’s disease diagnosis
The gastroenterologist would like to know about the patient's medical and family history, including medications, and jot down the patient's symptoms. The gastroenterologist would perform a thorough physical examination and would like to prescribe any or in combination of the following Crohn’s disease test.
- Blood test
- Stool test
- Intestinal endoscopy
- Capsule endoscopy
- Colonoscopy
- Upper GI endoscopy
- Balloon-assisted enteroscopy
- Upper GI series
- Computerised tomography
Crohn’s disease treatment
The treatment for Crohn's disease is still under research, where medication can help control or lessen the symptoms and prevent recurrence. The major forms of treatment are medications; however, occasionally, surgery may be required.
The medications include:
- Steroids
- Immunosuppressants
- Anti-inflammatory drugs
- Biological medicines
- Liquid diet
Surgery: The gastroenterologist will suggest surgery if the benefits are more in comparison to the risks. Surgery can aid in managing symptoms and prevent them from returning. Depending on the patient's condition, a gastro-surgeon can treat Crohn’s disease by the following surgical procedures:
- Small bowel resection
- Subtotal colectomy
- Proctocolectomy and ileostomy
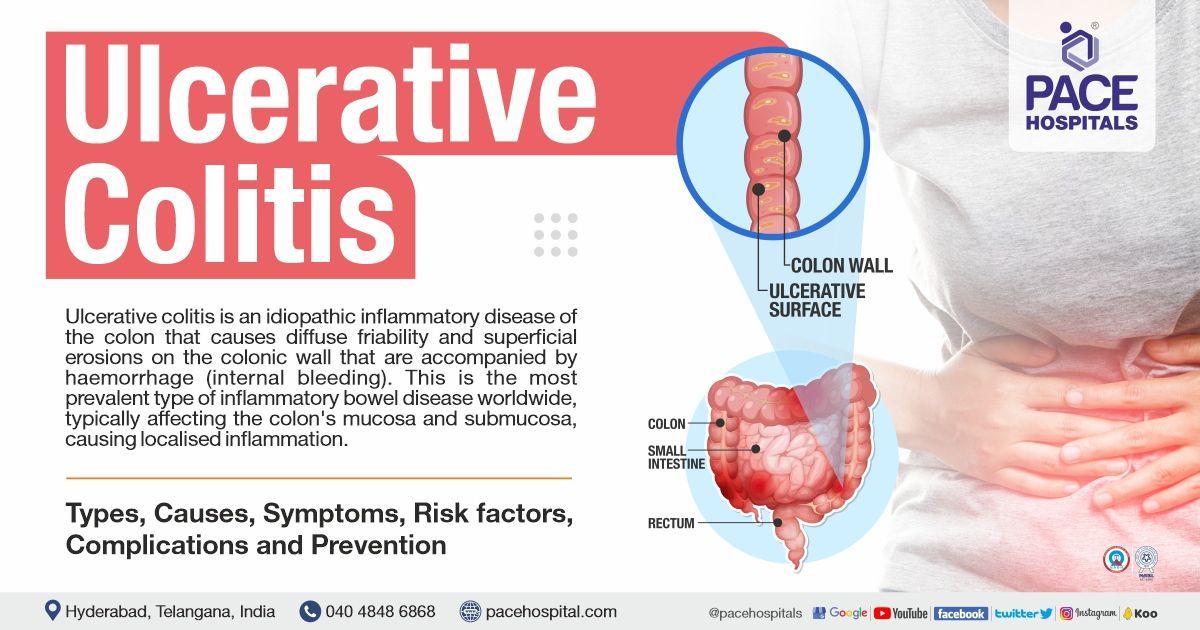
Difference between Ulcerative Colitis and Crohn's Disease
Both diseases affect the bowel in slightly different ways. Ulcerative colitis and Crohn’s disease difference are as follows:
| Elements | Ulcerative colitis | Crohn’s disease |
|---|---|---|
| Disease Location | Colon | Entire gastrointestinal tract (anywhere from the mouth to the anus) |
| Distribution | Complete and continuous inflammation of the colon | Inflammation occurs in between the healthy areas of the GI tract |
| Extent of damage | Only the innermost lining of the colon will be affected | It affects all the layers of the bowel wall (serosa to the mucosa) |
| Perianal disease, fistulae and stricture | Absent | Present |
| Prominent symptoms | Bloody diarrhoea, urgency in defecating, abdominal cramping, weight loss due to severe diarrhoea | Abdominal bloating, fissures with anal bleeding, weight loss due to severe diarrhoea |
Difference between Crohn's disease and Intestinal tuberculosis | Crohn's disease vs Intestinal tuberculosis
Crohn's disease and TB of the intestine are two chronic inflammatory diseases that can affect the gastrointestinal system. However, some significant distinctions between the two conditions are as follows:
| Elements | Crohn's disease | Intestinal tuberculosis |
|---|---|---|
| Fever Symptom | No specific pattern | Fever in evening with night sweats |
| Causes | Autoimmune diseases | Bacterial infection (Mycobacterium tuberculosis and Mycobacterium bovis) |
| Commonly affected area | Entire gastrointestinal tract; rectum, and terminal ileum | Ileocecal region, right colon, and ileum |
| Recurrence after surgery | Yes | Unlikely |
| Management | Continue immunosuppressive therapy | Short duration of therapy in compared to CD (anti-tubercular agents for 6 months) |
| Extraintestinal manifestations | More common | Less likely |
| Fistula formation | Common | Rare |
| Perianal disease | More common | Might present |
| Endoscopic findings | Skip lesions, Anorectal lesions, cobblestone appearance, longitudinal and aphthous ulcers | Circumferential ulcers, pseudopolyps, hypertrophic mucosa, and strictures |
| Clinical manifestations | Aphthous ulcers, fatigue, perianal disease, bloody stools, weight loss, and arthropathies | Fever, weight loss, abdominal pain, vomiting, loose stools, and night sweats |
Frequently Asked Questions - FAQs
-
Can Crohn’s disease be cured?
No, Crohn’s disease cannot be cured completely; however, providing patient-specific treatment can aid in managing its symptoms and reduce inflammations and complications to enhance long-term prognosis.
-
Is Crohn’s disease deadly?
Crohn’s disease is not a deadly disease. Nevertheless, improper management could lead to potential complications that may impact the patient's quality of life, resulting in fatal outcomes. With the right medical care and dietary adjustments, Crohn's disease does not pose a life-threatening hazard.
-
Is there a test for Crohn’s disease?
Yes, Crohn’s disease can be diagnosed by laboratory tests such as blood tests (anaemia & liver functions) and stool tests. It can also be identified by computerised tomography, colonoscopy, capsule endoscopy, balloon-assisted enteroscopy and magnetic resonance imaging.
-
What food to eat when you have Crohn’s disease?
The following are the food products, but not limited to are considered as Crohn’s disease diet, that need to be consumed by the patient.
- A diet rich in omega-3 fatty acids (omega-3s) such as walnut butter, flaxseed oil, fish (salmon, tuna) etc
- Fruits like bananas, blueberry, papaya, orange, grape
- Green leafy vegetables that include carrot, spinach, lettuce, green beans, capsicum
-
How to treat Crohn’s disease naturally?
A person with Crohn’s disease can adopt the following dietary practices that may get relief from their Crohn's disease symptoms:
- Drinking plenty of water
- Consume small and frequent meals (4- 6 times) in a day
- Boiled and grilled food supplements should be preferred rather than oily
- Consumption of low-fibre foods
-
Can a biopsy detect Crohn’s disease?
Yes, a biopsy detects Crohn’s disease if it is present in the areas of the large intestine. If the gastroenterologists suspect Crohn’s disease, he would like to prescribe colonoscopy or sigmoidoscopy. During these procedures, the gastroenterologists would collect a few samples of tissues from the lining of the patient's large intestine and send them for further lab analysis. The presence of inflammatory cell clusters in the sample collected signifies the diagnosis of Crohn’s disease.
-
Does Crohn’s disease cause back pain?
Yes, back pain is a common symptom of Crohn's disease; however, back pain without the presence of gastrointestinal tract symptoms would rule out the possibility of Crohn's disease as the cause of the back pain.
-
What is the latest treatment for Crohn's disease?
Stem cells have the capacity to reduce inflammation in the digestive tract and repair or regenerate the damaged tissue. The advancement of the disease can be downturn, and symptoms, including abdominal pain, diarrhoea, and weight loss, can be alleviated in addition to healing scar tissue in the large intestine. Relapses of Crohn's disease and perianal fistula that have not responded to conventional treatments may respond to stem cell therapy (SCT), according to preliminary research; however, more study is needed before SCT can be incorporated into clinical practice.
-
Can a blood test detect Crohn's disease?
Simple blood tests are not adequate for the diagnosis of Crohn's disease. However, blood tests are still crucial since they can help confirm a diagnosis and reveal changes in disease progression.
-
How does a gastroenterologist diagnose Crohn's disease?
Colonoscopy is the gold standard for diagnosing Crohn's disease. The gastroenterologist can check for inflammation, ulcers, and other indicators of intestinal bowel disease (IBD) in the intestinal lining using live video pictures of the colon and rectum through the colonoscope. In addition, a small sample (biopsy)of colon tissue is removed for laboratory analysis, which is a common part of a colonoscopy procedure. The results of a biopsy can assist in confirming a diagnosis of Crohn's disease and distinguish between other IBD diseases.
-
When should you get checked for Crohn's disease?
One should visit gastroenterologists immediately when they have observed any changes in bowel habits that don't go away or experiencing any of the following symptoms of Crohn's disease as:
- Pain in the abdomen
- Rectal bleeding
- Vomiting and its sensations
- Increase in body temperature
- Prolong diarrhoea (more than two weeks)
- Weight loss
Related article

Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.

Our Locations
Subscribe to our newsletter and stay updated with the latest health information.
By clicking on subscribe now, you accept to receive communications from PACE Hospitals on email, SMS and Whatsapp.
Subscribe to PACE Hospitals News
Thank you for subscribing. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
-

Payment in advance for treatment (Pay in Indian Rupees)
For Bank Transfer:-
Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545
Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc)
Call us at 04048486868
ADDRESS
PACE Hospitals
Hitech City : Beside Avasa Hotel, Pillar No. 18, Hyderabad - 500081
Madinaguda: Mythri Nagar, Beside South India Shopping, Madinaguda, Hyderabad - 500050
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals as such.