Advancing Tissue Assessment with Near-Infrared Imaging: What is the Difference Between Oxygenation and Perfusion?
Oxygen is critical to life.
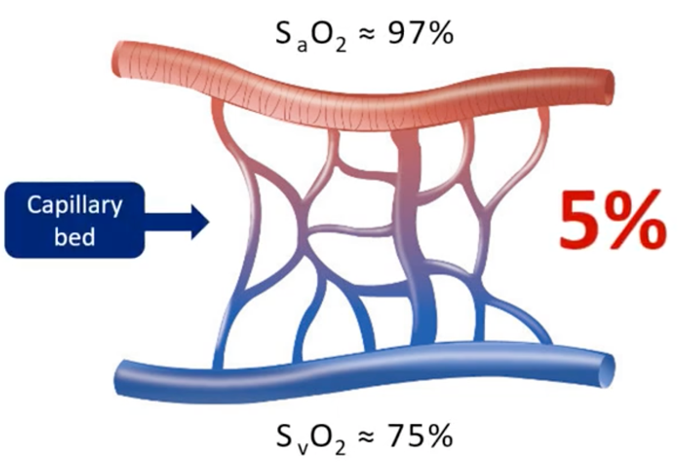
The delivery and utilization of oxygen at the cellular level is the primal determinant of the viability of cells and the tissue structures they support. The capillary beds, between the arterial supply and the venous return, contain approximately 5% of our total blood volume. It is in these capillaries where gas, nutrients and waste exchange occur between the cells and the bloodstream.
What is the difference between Perfusion and Oxygenation?
Oxygenation and perfusion display a non-linear relationship. Oxygenation (StO2) begins to drop when cellular demand is greater than blood oxygen supply. Oxygenation measure the balance between local oxygen supply and demand. Essentially stating a person can have low perfusion but still have well oxygenated tissue meeting the functional demand of the soft tissue being analyzed. Conversely, there can be adequate perfusion in the large vessels, but poor oxygen exchange in the capillary network. While arterial oxygen, arterial flow and large vessel patency are both important and necessary for sustaining cellular viability, they are not sufficient conditions for ensuring cellular viability.
Most of the commercially available technologies provide indirect or surrogate measures for tissue viability, measuring perfusion but not oxygenation at the critical microvascular level.
Blood flow measuring techniques, such as laser doppler, provide a measure of perfusion, but they are largely indicative of the arterial flow. Pulse oximetry provides a hemoglobin oxygen saturation, an SpO2, that is strongly correlated with the SaO2, or the hemoglobin arterial oxygen saturation. Both technologies focus on the arterial supply only.
Angiographic methods, such as ICG fluorescence imaging, were developed to determine the patency of the conduit or larger vessels.
The technologies discussed are all inferential and provide indicators that the cells and the tissue are receiving an adequate supply of oxygen and nutrients for survival, only indirectly.
Image credit: M. Sowa, PhD.
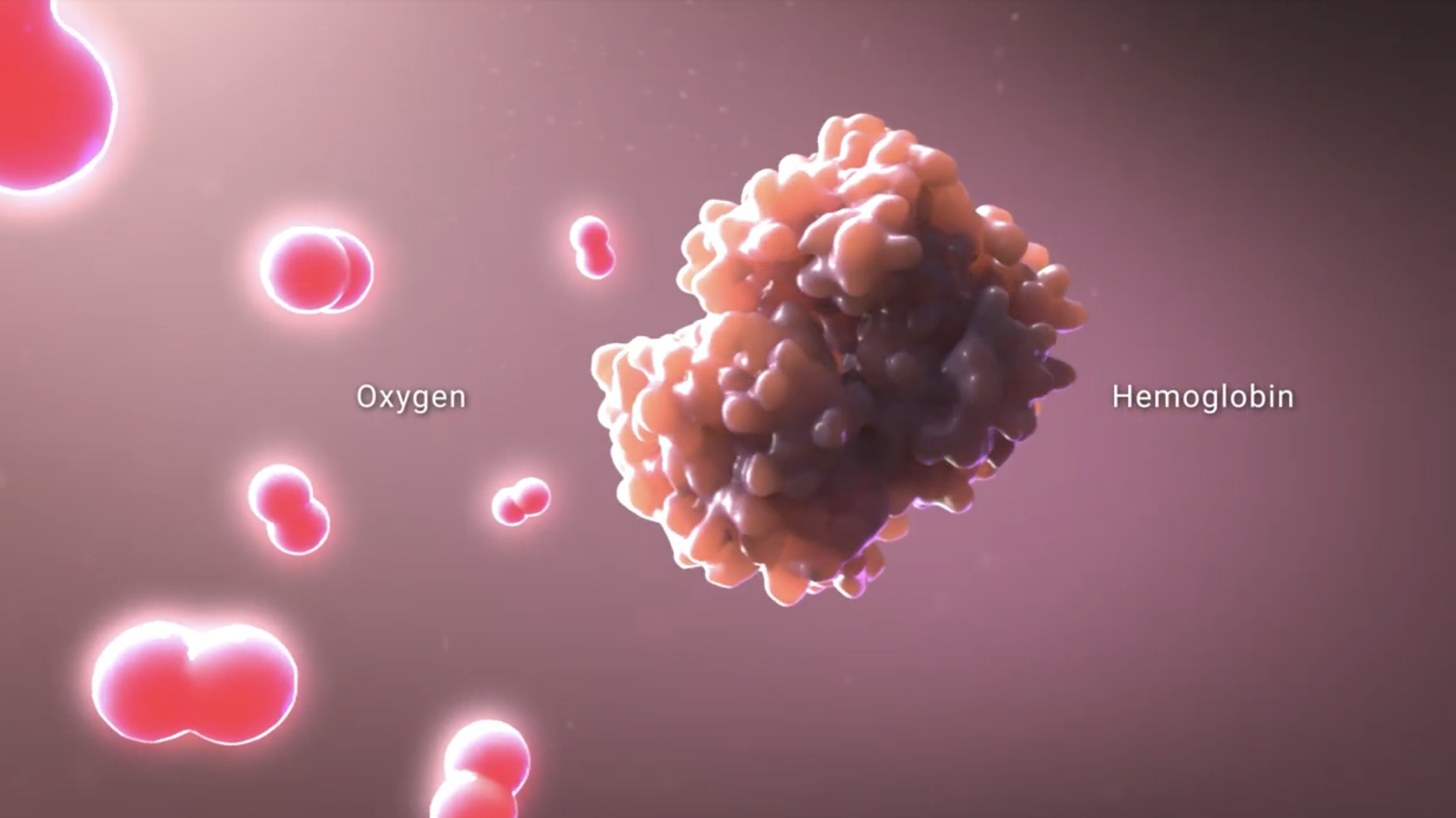
Oxygen is transported from the oxygen-rich environment of our lungs to the periphery by red blood cells. These red blood cells contain millions of hemoglobin molecules that reversibly bind to the oxygen that diffuses into them. The optical properties of hemoglobin change when hemoglobin binds to oxygen. Therefore, one can use light to determine whether oxygen is bound or unbound from hemoglobin.
How does near-infrared spectroscopy measure the critical microvascular network?
Near-infrared spectroscopy (NIRS) imaging takes a closer step to measuring cellular respiration. With this technology, one can measure hemoglobin oxygenation at the tissue/cellular interface, a measurement referred to as tissue oxygen saturation or StO2.
Near-infrared spectroscopy imaging provides a non-invasive measure of the content of oxygen bound to hemoglobin in the blood, just below the surface of the tissue being imaged. Unlike other technologies, NIRS is not restricted to looking at either arterial supply or venous return. Instead, NIRS provides a comprehensive measure of the hemoglobin oxygenation of the entire vascular bed, including the nutritive vascular bed.
By measuring the tissue hemoglobin oxygen saturation, NIRS imaging with SnapshotNIR provides the user with actionable data on both the oxygen delivery and oxygen extraction at the critical cellular level. With this innovative technology, one can determine areas where oxygen delivery is not meeting local metabolic demand. Detection and delineation of these areas of critical hypoxia provide a better assessment of tissue viability and translates into enhanced clinical decision making, forging a new path in diagnostic driven wound care. SnapshotNIR documents healing progression and helps clinicians to positively impact patient outcomes and reduce complications.
See the science behind SnapshotNIR here.
References:
EO2 Concepts, Coffee with Clinicians with Amanda Killeen, DPM
https://www.youtube.com/watch?v=ObYKBYvYHrY
Hyperspectral imaging for early detection of oxygenation and perfusion changes in irradiated skin, 2012, Michael S. Chin, Brian B. Freniere, Yuan-Chyuan Lo, Jonathon H. Saleeby, Stephen P. Baker, Heather M. Strom, Ronald A. Ignotz, Janice F. Lalikos, Thomas J. Fitzgerald https://www.spiedigitallibrary.org/journals/journal-of-biomedical-optics/volume-17/issue-2/026010/Hyperspectral-imaging-for-early-detection-of-oxygenation-and-perfusion-changes/10.1117/1.JBO.17.2.026010.full?SSO=1
Review of near-infrared methods for wound assessment, January 2016, Journal of Biomedical Optics 21:091304, Michael G. Sowa, Wen-Chuan Kuo, Alex C-T. Ko, David G. Armstrong, https://www.researchgate.net/publication/301355168_Review_of_near-infrared_methods_for_wound_assessment