Bildtitel
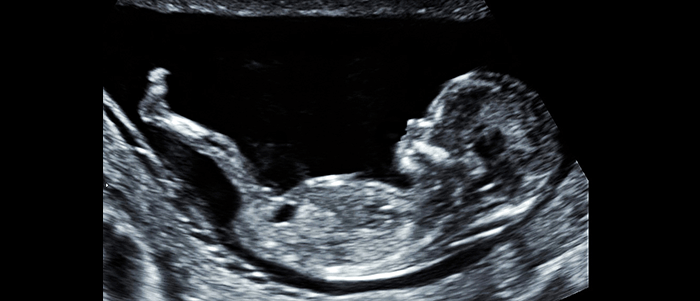
The fetus at first trimester screening (2D)
Button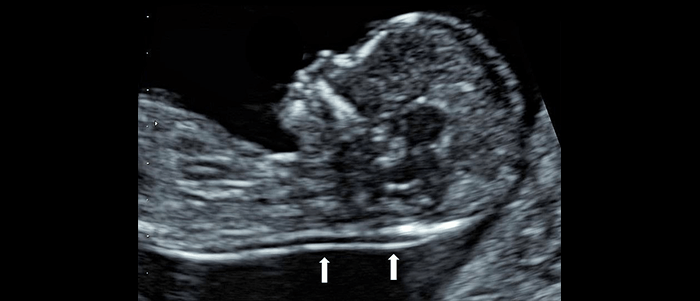
Bildtitel
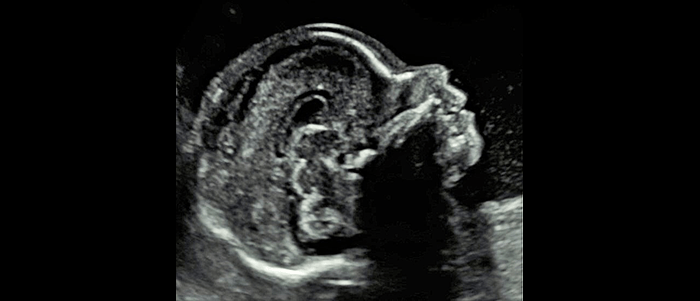
Nuchal translucency and fetal profil
Button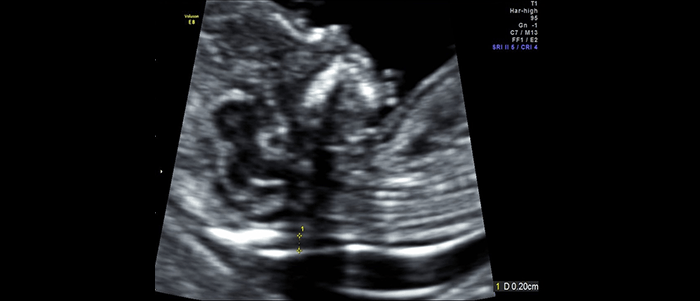
Bildtitel
Nuchal translucency (normal) and nasal bone
Button
Bildtitel
The fetus at first trimester screening (3D)
Button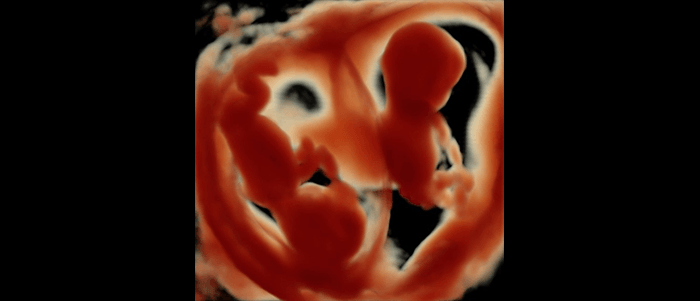
Bildtitel
Twins (3D)
Button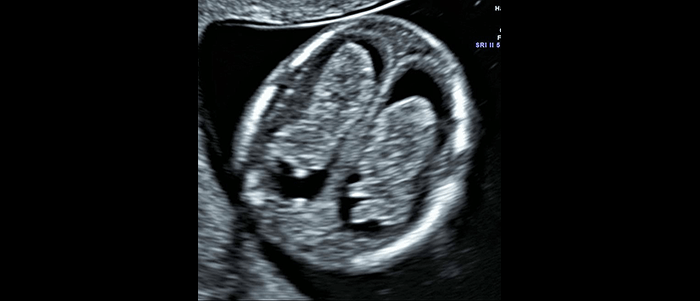
Bildtitel
Head and brain (normal)
Button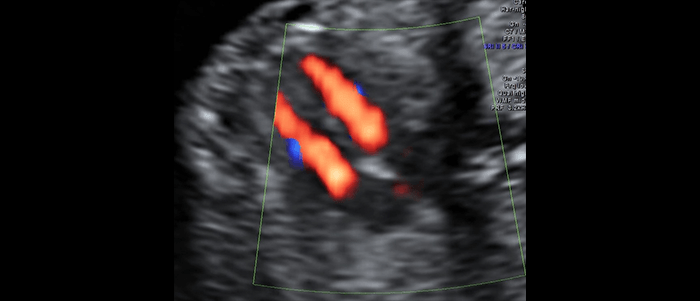
Bildtitel
Heart. Four chamber view
Button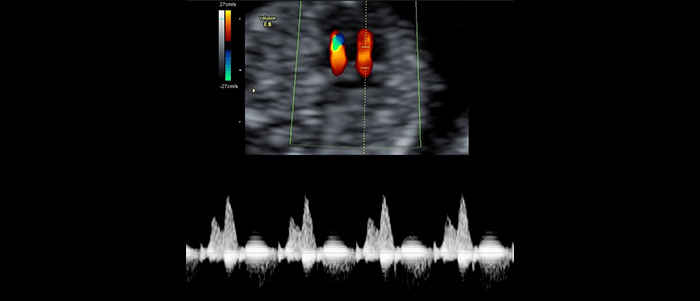
Bildtitel
Normal blood flow at the tricuspid valve
Button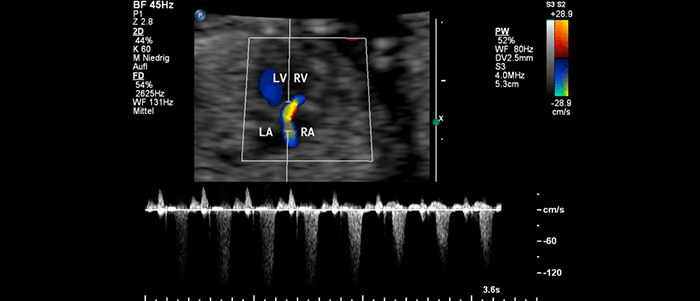
Bildtitel
Abnormal blood in the ductus venosus
Button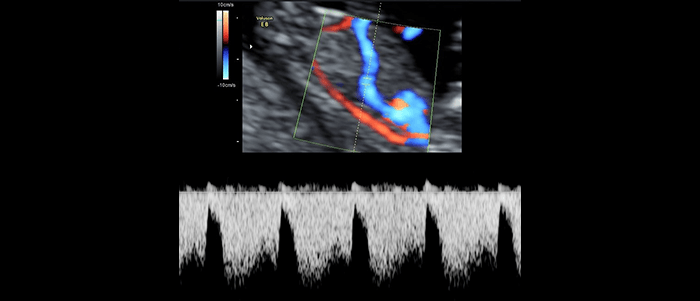
Bildtitel
Normal blood flow in the ductus venosus
Button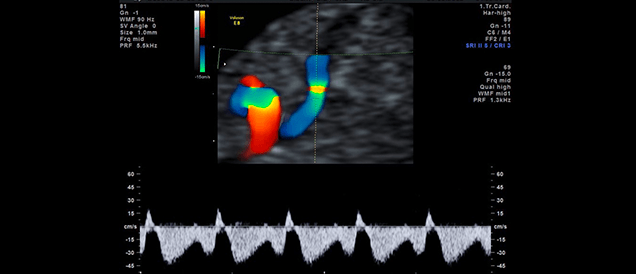
Bildtitel
Abnormal blood in the ductus venosus
Button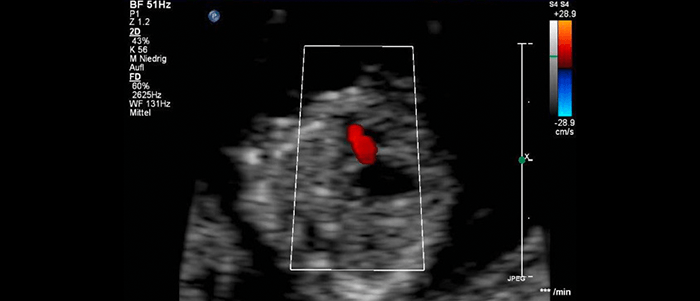
Bildtitel
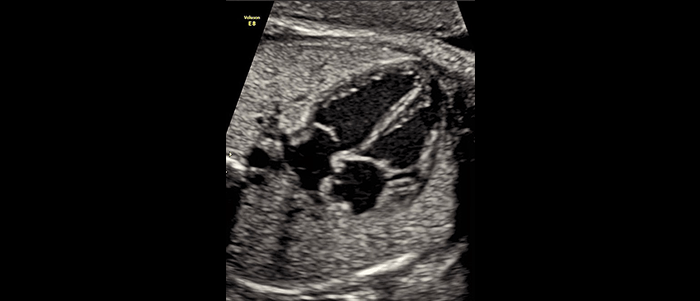
Heart defect at first trimester screening
Button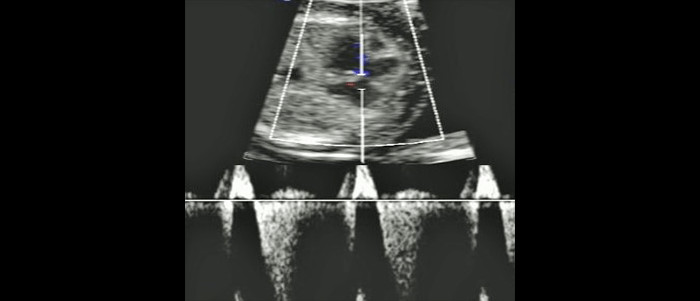
Bildtitel
Heart defect in early pregnancy (atrioventricular septal defect)
Button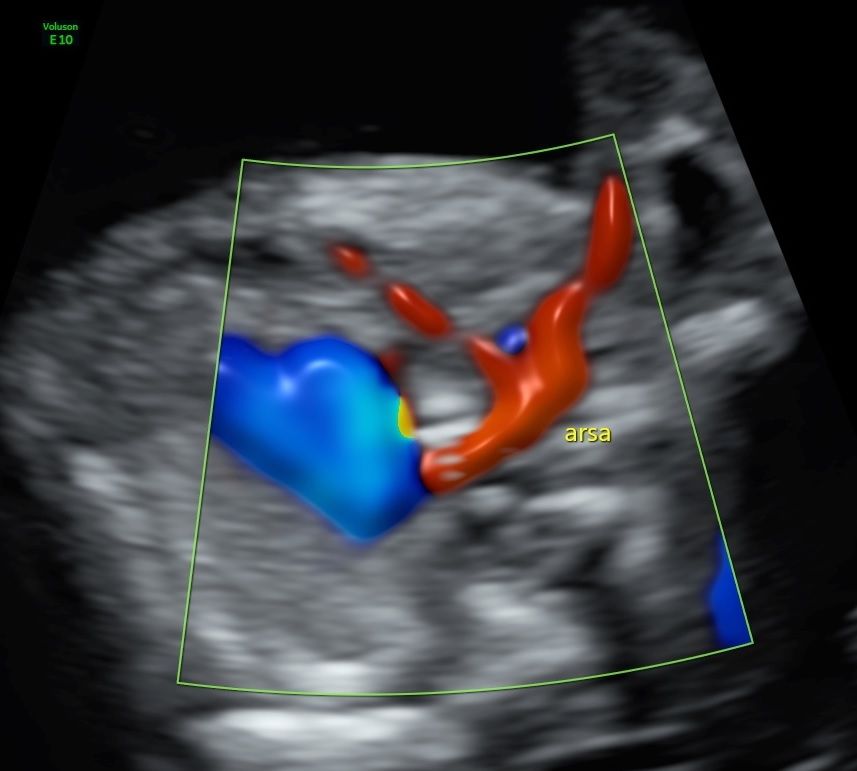
Bildtitel
Aberrant right subclavian artery
Button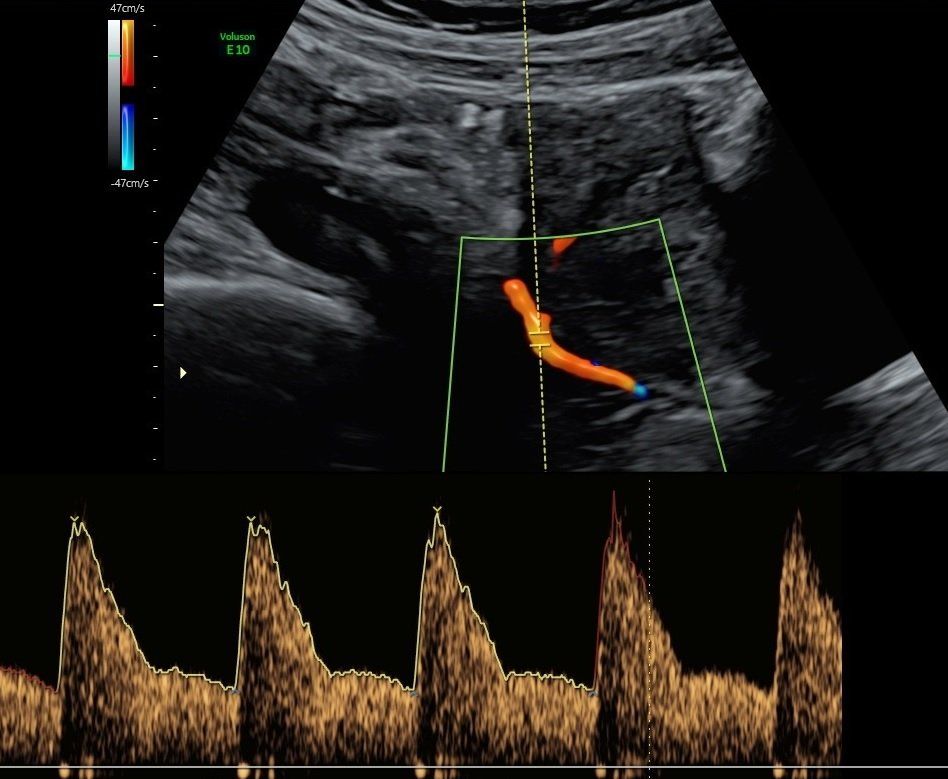
Bildtitel
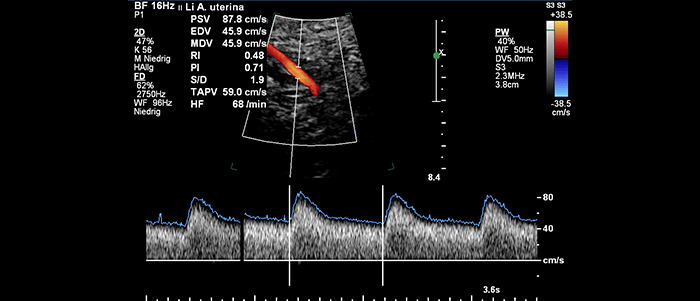
Dopplersonography of the uterine artery
Button
Bildtitel
3D first trimester
Button
First-trimester screening, screening for pre-eclampsia
First-trimester screening is a noninvasive, risk-free procedure (ultrasound examination combined with maternal blood sample) which is conducted in the early part of pregnancy to assess the individual risk of the presence of chromosomal disorders (trisomy 13, 18, 21) in the fetus.
We recommend that the blood sample for first-trimester screening be taken several days before the ultrasound examination. The results are then available when the ultrasound examination is performed so that the findings can be conclusively discussed.
In calculating the risk, the factors taken into consideration are maternal age, two laboratory values (free ß-HCG and PAPP-A produced by the placenta) from the maternal blood, the thickness of the nuchal fold in the fetus (nuchal translucency, NT) measured on ultrasound and further ultrasound parameters (e.g., nasal bone, tricuspid valve blood flow).
On ultrasound examination, the extent of an accumulation of fluid in the fetal neck (nuchal translucency, NT) is measured. Minimal nuchal translucency is normal. As the thickness increases, so does the risk of chromosomal abnormalities and other diseases.
The test result is given as an individual probability for the presence of the most frequent chromosomal abnormalities (trisomy 13, 18, 21). If the risk is low (e.g., 1:2000), the test result is considered normal. In such cases, the low risk is usually accepted, and no invasive diagnostic test is undertaken (amniocentesis, chorionic villus sampling). A further reduction of the risk for the most frequent chromosomal abnormalities is possible by performing the non-invasive prenatal test ( see NIPT).
If the risk of chromosomal abnormalities is higher (e.g. 1:50), the test result is considered abnormal. The test results demonstrate an increased risk of chromosomal abnormalities in about 3%-5% of all first-trimester screening examinations conducted and in approximately 90%-97% of pregnancies with chromosomal abnormalities, depending on the quality and the extend of the ultrasound examination.
In cases of higher risk, parents usually want certainty about the presence or absence of a chromosomal abnormality. This is then provided by amniocentesis (examination of the amniotic fluid) or chorionic villus sampling (sampling the placental tissue).
First-trimester screening can only be performed between the 12th (11+) and 14th (13+) weeks of pregnancy since the accumulation of fluid behind fetal neck is a temporary effect which only exists between about weeks 10 and 15. Since increased nuchal translucency thickness can also be associated with other developmental problems (such as heart defects), it is advisable in such cases to undergo further ultrasound diagnosis of malformations (see below) in addition to chromosomal analysis.
During ultrasound examination in first-trimester screening, we also perform an early diagnosis of anomalies, which permits us to detect other developmental problems in the fetus. This early anomaly diagnosis does not, however, in any way constitute a satisfactory substitute for the more advanced ultrasound diagnosis of organic anomalies (e.g., heart defects, brain malformations), which is usually advisable between the 20th and 22nd weeks of pregnancy (high-resolution ultrasound, anomaly diagnosis, DEGUM II/III ultrasound).
Early diagnosis of malformation and measurement of nuchal translucency thickness require high-resolution ultrasound equipment as well and time and experience on the part of the examiner. The ultrasound and laboratory examinations are certified by the Fetal Medicine Foundation (FMF) London and the German FMF, and are annually re-examined. We hold certificates of competence for all currently available ultrasound measurements of the Fetal Medicine Foundation (nuchal transparency, nasal bone, tricuspid flow, ductus venosus flow).
Screening for pre-eclampsia
At first trimester screening we also estimate the risk for the occurence of preeclampsia and placental insufficency. In case of an increased risk preventive treatments may improve pregnancy outcome.
In the further course of the pregnancy, the first-trimester screening can by supplemented by the non-invasive prenatal test (NIPT) and a high-resolution ultrasound scan in the 20th to 22nd week of pregnancy.
Non-invasive prenatal diagnostics: Diagnosis of malformations by ultrasound & non-invasive prenatal test NIPT for the unborn baby
Already during pregnancy, abnormalities in the fetus can be detected by non-invasive prenatal diagnostics using ultrasound, Doppler sonography, fetal echocardiography and the non-invasive prenatal test NIPT. At the Prenatal Centre Stuttgart Prof. Dr. Mielke / Dr. Bosselmann we offer you the possibility of having the entire diagnostic procedure carried out in accordance with the standards of the German Society for Ultrasound in Medicine (DEGUM II/III) and the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG).
With the following overview, you can find out about non-invasive prenatal diagnostics and the non-invasive prenatal test NIPT at the Prenatal Centre Stuttgart Prof. Dr. Mielke / Dr. Bosselmann.
What is non-invasive prenatal diagnostics & what tests does it include?
Depending on the week of pregnancy you are currently in, special screening examinations can be carried out. For example, you can take advantage of the first trimester screening in the 12th to 14th week of pregnancy. This early pregnancy examination with ultrasound is non-invasive and produces high-resolution images of your child. In this way, the timely development of the organs and growth can be assessed. Non-invasive prenatal diagnosis by ultrasound also provides information on the development of the amniotic fluid, placenta and umbilical cord blood flow. In addition, there may be indications of chromosomal disorders such as trisomy 13, trisomy 18 and trisomy 21.
An indication of an abnormality in the development of the foetus can be an increased accumulation of fluid in the neck of the child (increased nuchal translucency). While a small accumulation of such fluids is normal, an increased accumulation may be associated with a chromosomal disorder or other diseases. Further clarification can be done by ultrasound (fine ultrasound, organ ultrasound, Doppler sonography, fetal echocardiography), the non-invasive prenatal test NIPT or invasive procedures such as amniocentesis or placenta tissue sampling.
What is a non-invasive prenatal test NIPT?
A non-invasive prenatal test (NIPT) is a further examination in which the mother's blood is examined. We can carry out this test for you at the Prenatal Centre Stuttgart Prof. Dr. Mielke / Dr. Bosselmann. This is a patented procedure in which the genetic material (cell-free DNA) of the placenta is examined. The non-invasive prenatal test NIPT at the Prenatal Centre Stuttgart Prof. Dr. Mielke / Dr. Bosselmann is a supplementary examination to the already mentioned examinations with regard to chromosomal disorders. Placental cell-free DNA can be detected in maternal blood with this procedure. The test has high detection rates for the most common chromosomal disorders such as trisomy 21, trisomy 13 and trisomy 18 and can be carried out in addition to the DEGUM II/III ultrasound examinations, which should usefully precede the blood collection for a non-invasive prenatal test NIPT at the Prenatal Centre Stuttgart Prof. Dr. Mielke / Dr. Bosselmann.
What further examinations are possible in the diagnosis of malformations?
A non-invasive prenatal test NIPT has already been carried out in Stuttgart? In addition to the above-mentioned examinations in early pregnancy, you can preferably take advantage of further examinations between the 20th and 22nd week of pregnancy. These include ultrasound examinations (fine ultrasound, organ ultrasound) according to DEGUM II/III, Doppler sonography (assessment of blood flow e.g. to the umbilical cord) and fetal echocardiography (diagnosis of heart defects).
Non-invasive prenatal diagnostics from specialists
Whether you opt for the non-invasive prenatal test NIPT, first trimester screening, fine ultrasound, Doppler sonography or fetal echocardiography: Our team of specialists at the Prenatal Centre Stuttgart Prof. Dr. Mielke / Dr. Bosselmann is there for you and will advise you in detail in advance.
Make your personal appointment now!
Non-invasive prenatal test (NIPT)
Test on placental cell-free DNA in maternal blood (e.g. Harmony Test®, Panorama Test®, PraenaTest®)
Test on placental cell-free DNA in maternal blood (e.g. Harmony Test®, Panorama Test®, PraenaTest®)
The test on placental cell-free DNA (genetic material) in maternal blood, offered in Germany since 2012, is an addition to the possibilities of non-invasive prenatal diagnosis in terms of the most common chromosomal abnormalities. With the NIPT, a high proportion, but not all cases of trisomy 13, 18 and 21 as well as a high proportion of the abnormalities in the number of sex chromosomes can be detected. Currently, additional applications are offered. It can rarely happen that there is a false positive finding or that the evaluation of the blood sample fails. NIPT is not an alternative to the first-trimester screening (ultrasound diagnosis) or amniocentesis or chorionic villus sampling (reliable detection or exclusion of all chromosomal abnormalities), but a supplement to the non-invasive tests with very high detection rates for the most common chromosomal abnormalities. A positive finding with the NIPT must be confirmed by an invasive diagnostic procedure (amniocentesis or chorionic villus sampling).
If you consider to use the NIPT, we recommend that it should be preceded by a first-trimester screening for a qualified early ultrasound examination. Ultrasound abnormalities may be due to a variety of genetic and non-genetic diseases which are not detectable with the NIPT.
Bildtitel
Normal brain (sagittal scan)
Button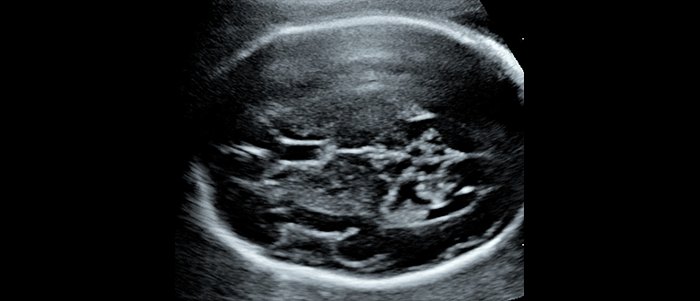
Bildtitel
Imaging of the normal brain (axial scan)
Button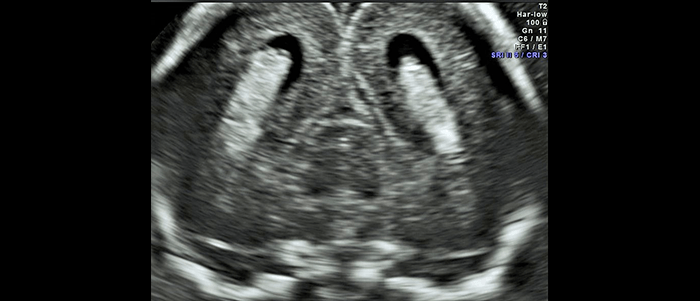
Bildtitel
Fetal brain (coronal scan)
Button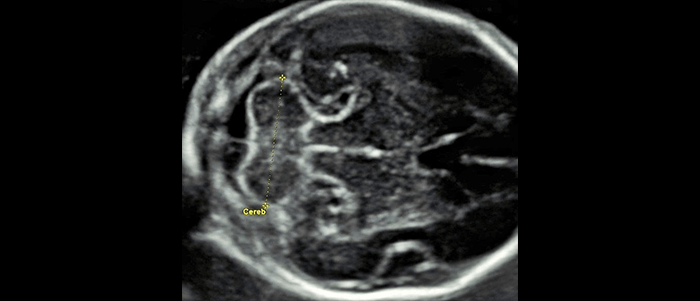
Bildtitel
Cerebellum
Button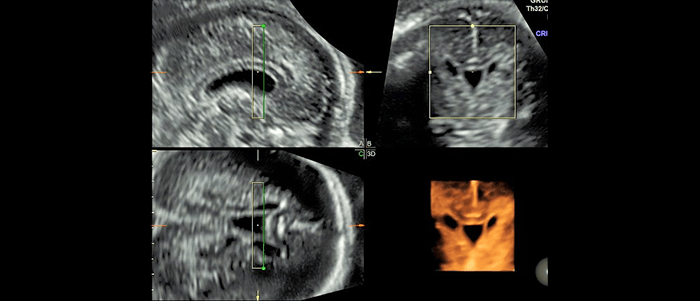
Bildtitel
Normal brain (3D)
Button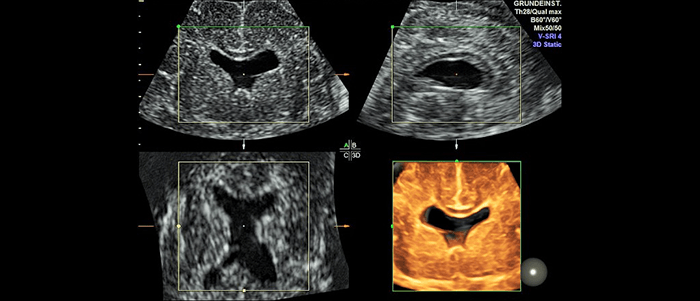
Bildtitel
Midline defect of the brain (3D)
Button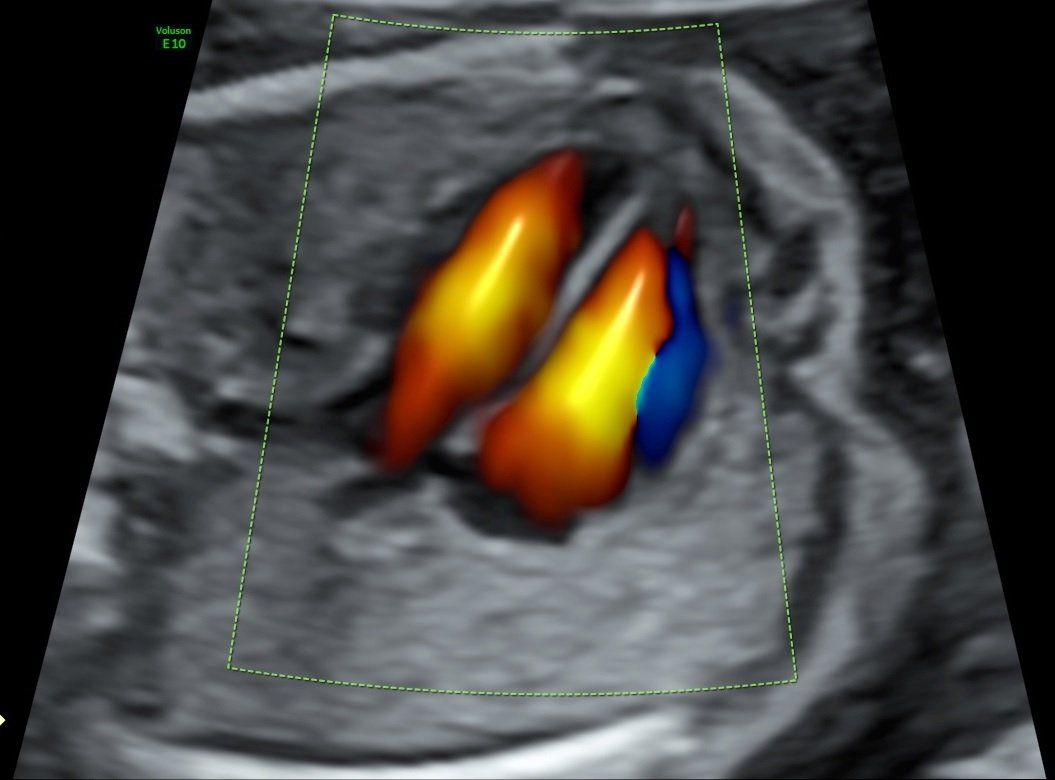
Bildtitel
Heart. Four chamber view
Button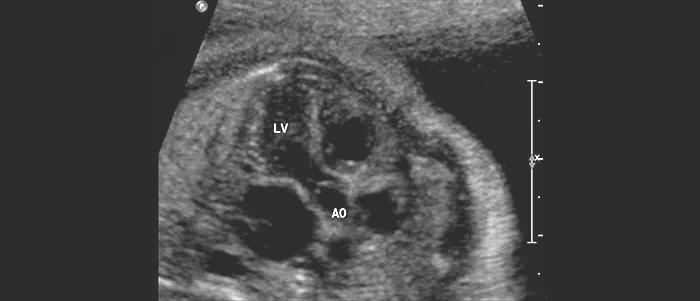
Bildtitel
The fetal heart. Five chamber view
Button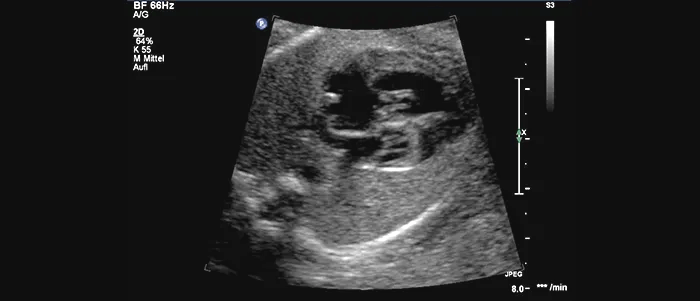
Bildtitel
Severe heart defect. Hypoplastic left heart
Button
Bildtitel
The fetal leg
Button
Bildtitel
The fetal foot
Button
Bildtitel
Male genitalia
Button
Bildtitel
Myoma of the uterus
Button
Bildtitel
Shortening of the cervix
Button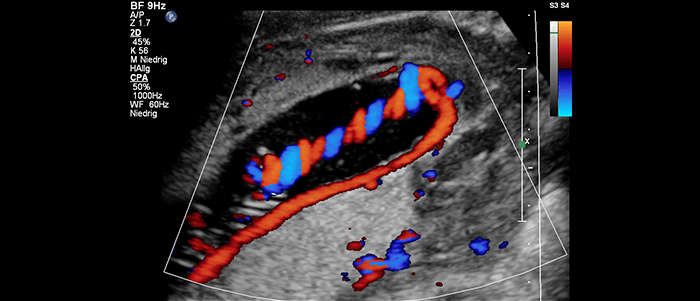
Bildtitel
Insertion anomaly of the umbilical cord
Button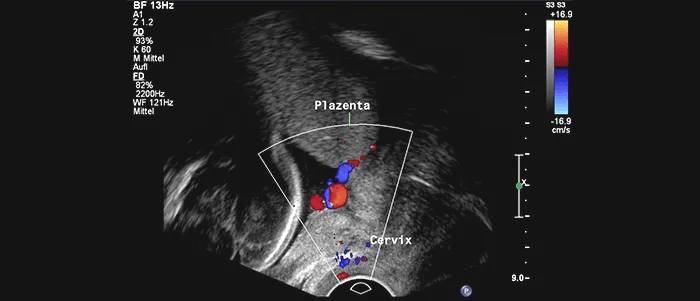
Bildtitel
Vasa previa
Button
Bildtitel
The fetal profile
Button
DEGUM II/III ultrasound scan in the 20th-22nd week of pregnancy (Organ diagnosis, anomaly diagnosis)
In an advanced, high-resolution ultrasound scan which is usually advisable between the 20th and 22nd week of pregnancy, a wide range of fetal developmental anomalies and organ malformation can be diagnosed, some of which are not recognizable in the early stages of pregnancy.
Prenatal diagnosis of congenital anomalies is often very significant for the further course of the pregnancy, birth and the neonatal phase (see below: options, limits and the consequences of prenatal diagnosis). This is particularly true for heart defects (see fetal echocardiography).
In the course of this high-resolution ultrasound scan, the uterus, placenta and amount of amniotic fluid are also assessed. Furthermore, Doppler sonography, fetal echocardiography and – if possible – 3D ultrasound are conducted (as far as the examination conditions permit).
Bildtitel
Normal placental circulation
Button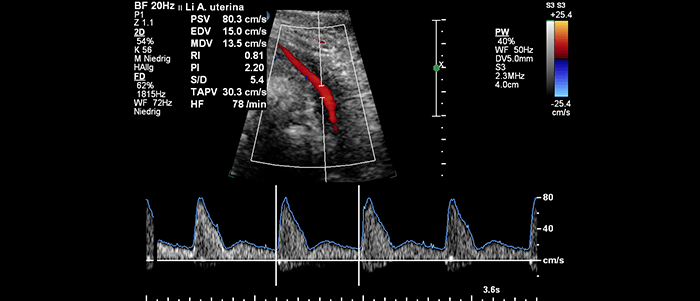
Bildtitel
Abnormal blood flow of the placental circulation
Button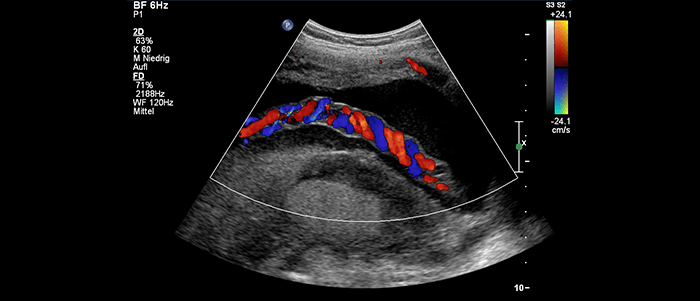
Bildtitel
Umbilcal vessels
Button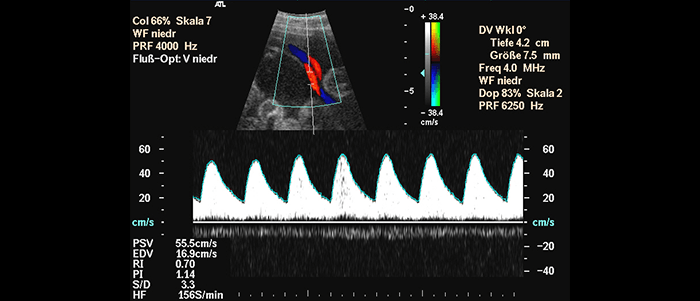
Bildtitel
Normal bood flow in the umbilical artery
Button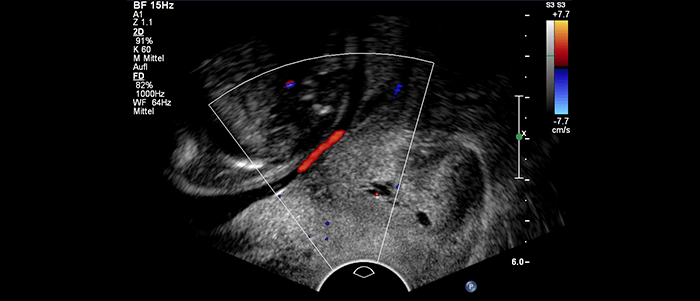
Bildtitel
Aberrant umbilical vessel at the internal orifice of the uterus
Button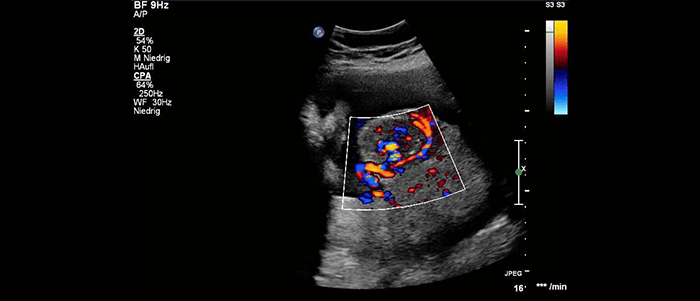
Bildtitel
Vascular tumor of the placenta (chorioangioma)
Button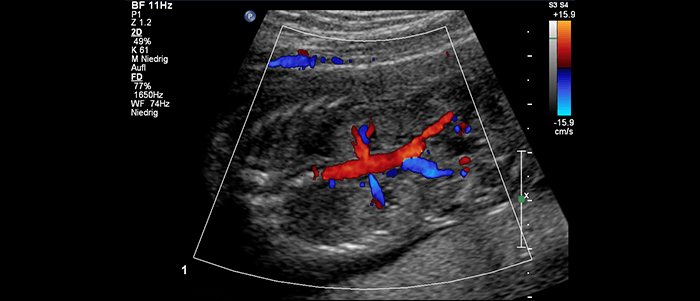
Bildtitel
Both kidneys and Color Doppler imaging of the renal vessels
Button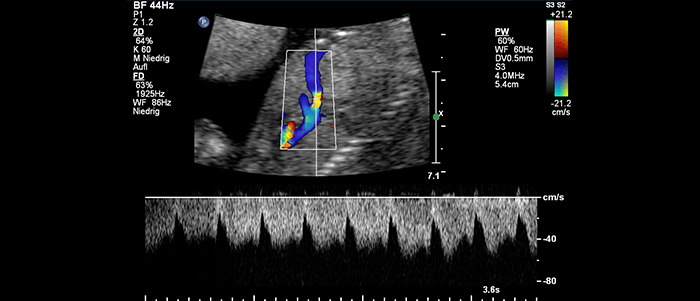
Bildtitel
Doppler sonography of the ductus venosus
Button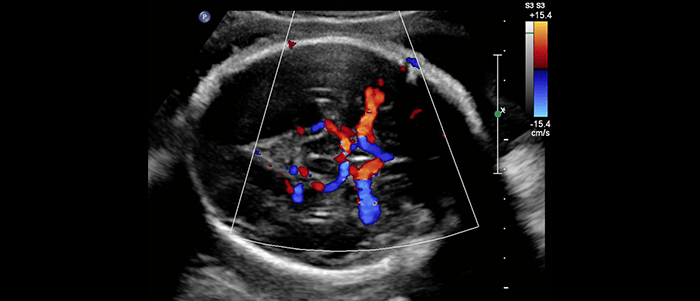
Bildtitel
Circulation of the fetal brain
Button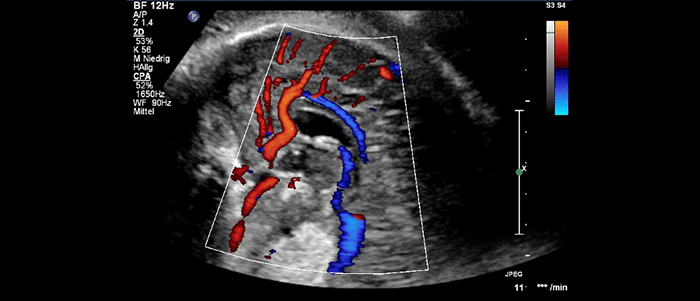
Bildtitel
Circulation of the fetal brain (pericallosal artery)
Button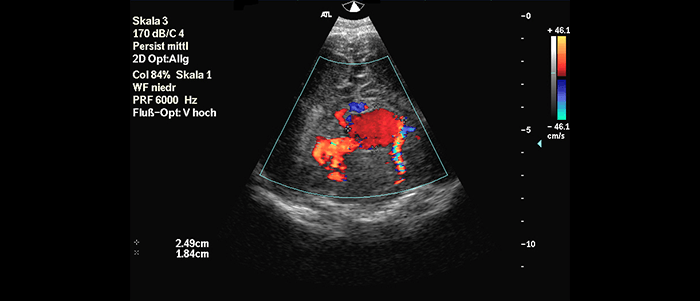
Bildtitel
Fetal brain. Vein of galen aneurysmal malformation
Button
Doppler sonography
Using Doppler sonography, a special ultrasound procedure for showing and measuring the blood circulation, it is possible to measure the blood supply to the uterus and placenta and in the umbilical cord, and the blood circulation in the unborn child. From these data, one can evaluate the blood supply to the fetus and the functional status of its heart and circulation as well as identify risks. Color-coded Doppler sonography (color Doppler) provides an improved diagnosis of placental and umbilical cord abnormalities and fetal malformations, particularly the diagnosis and differentiation of heart defects (fetal echocardiography).
Bildtitel
The fetal heart. Four chamber view
Button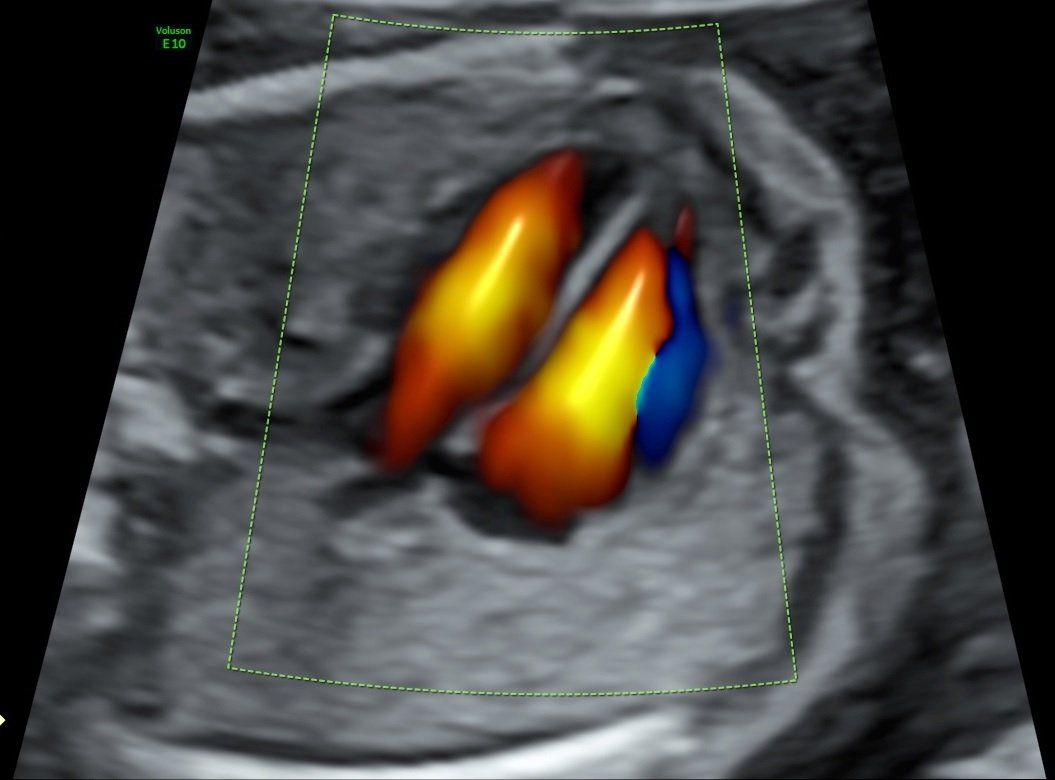
Bildtitel
Four chamber view. Color Doppler imaging
Button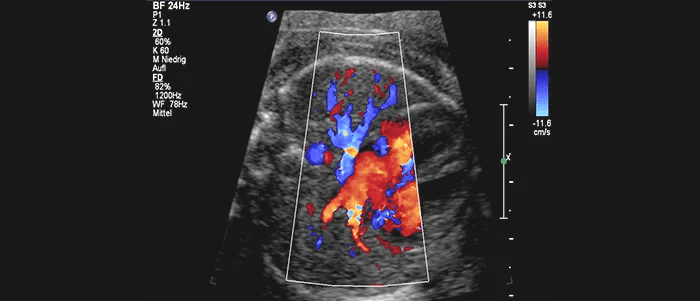
Bildtitel
Pulmonary veins
Button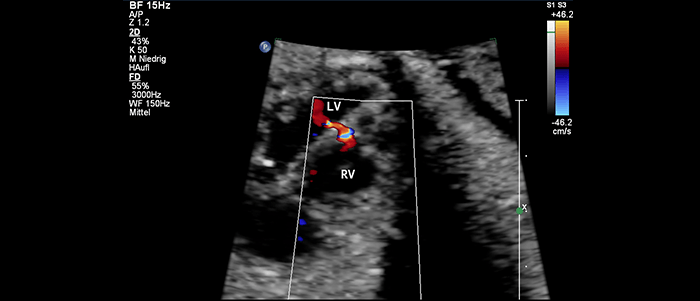
Bildtitel
Ventricular septal defect
Button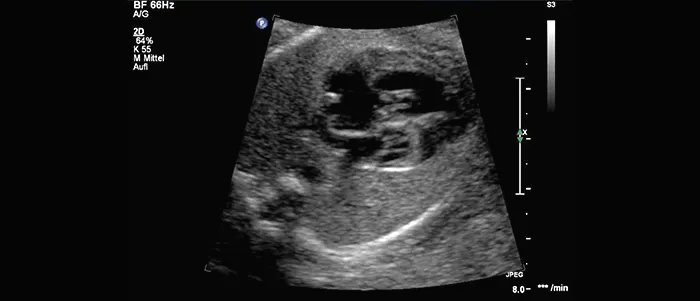
Bildtitel
Severe heart defect. Hypoplastic left heart syndrome
Button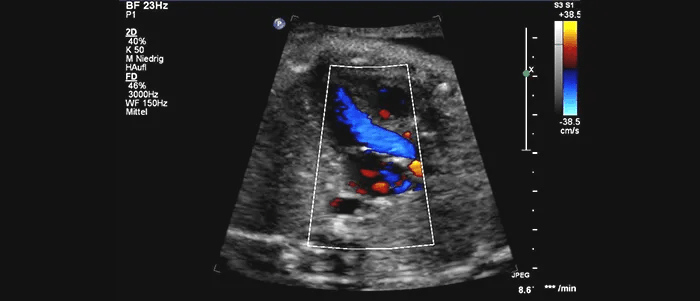
Bildtitel
Five chamber view. Color Doppler imaging
Button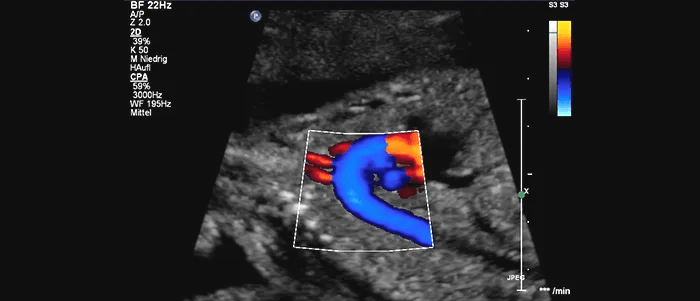
Bildtitel
Aortenbogen
Button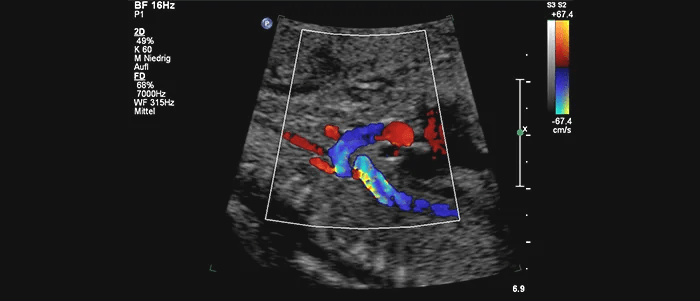
Bildtitel
Heart defect. Stenosis of the aortic arch
Button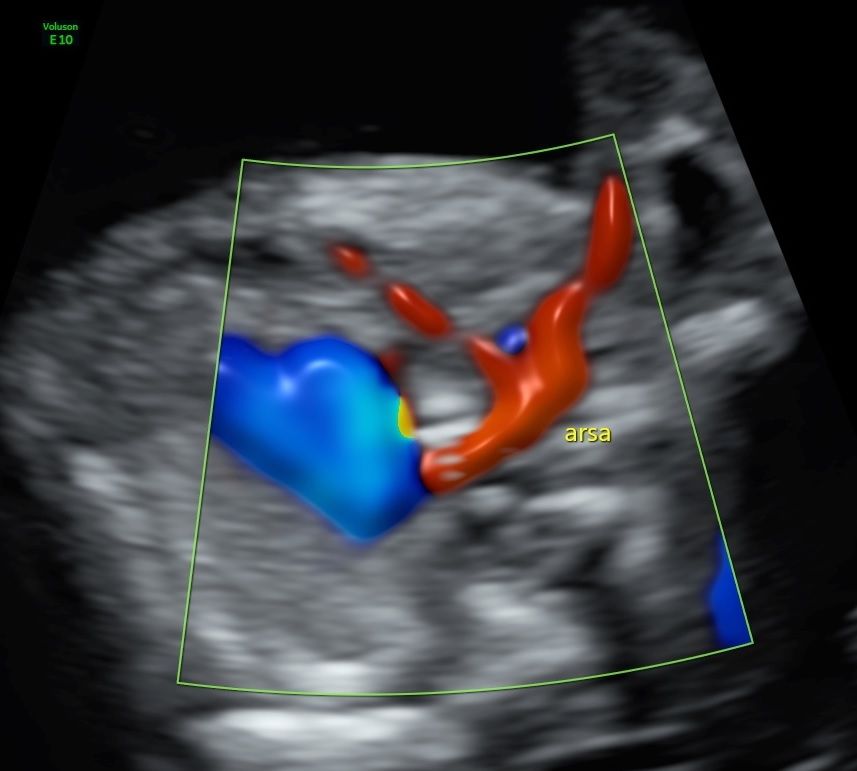
Bildtitel
Aberrant right subclavian artery
Button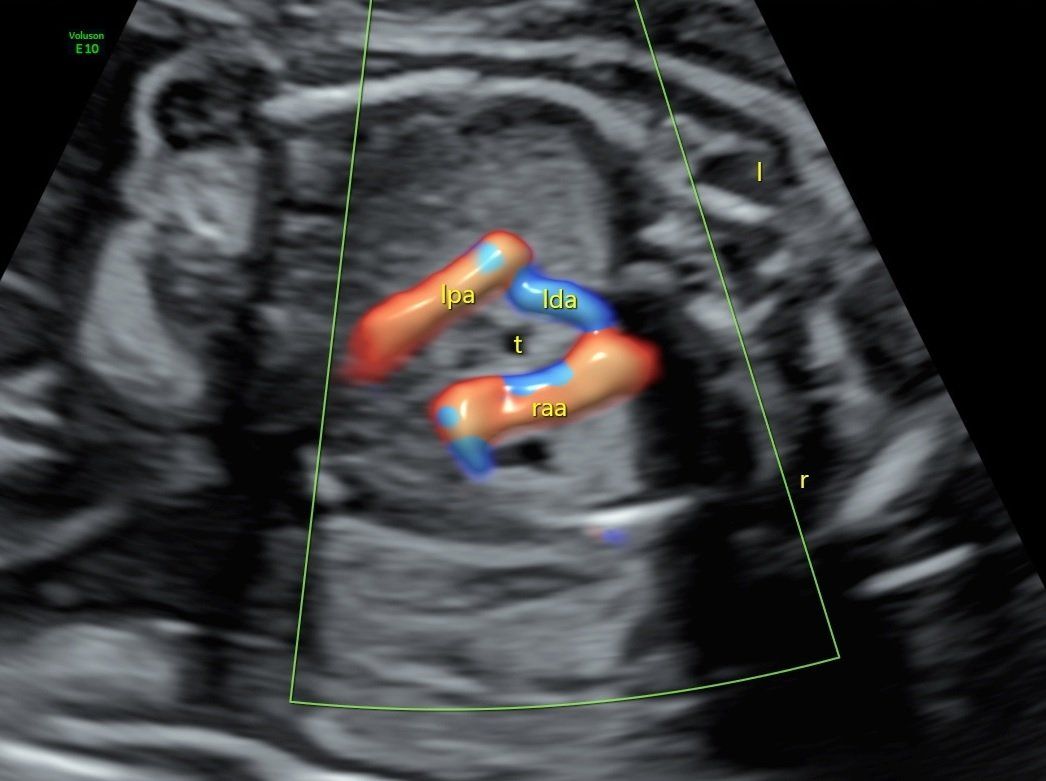
Bildtitel
Right aortic arch
Button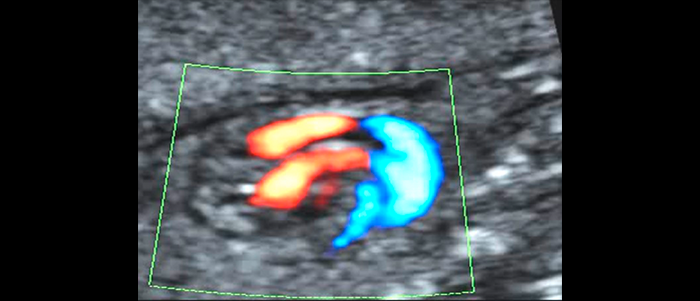
Bildtitel
Tranposition of the great arteries
Button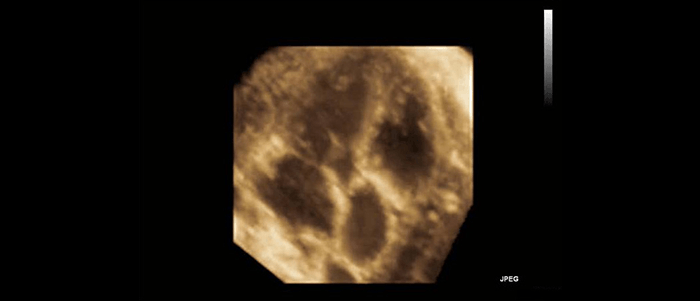
Bildtitel
3D echokardiography. Aortic valve stenosis
Button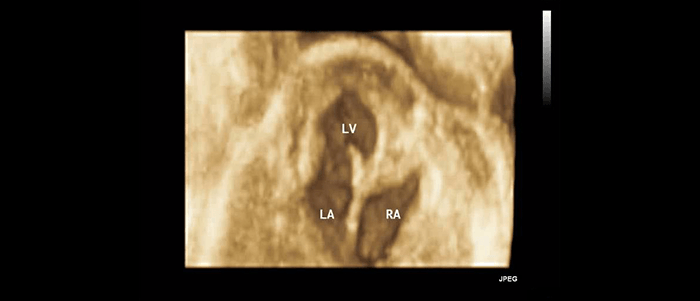
Bildtitel
3D echocardiography. Tricuspid valve atresia
Button
Fetal echocardiography
Fetal echocardiography describes a special ultrasound examination of the heart using two-dimensional and Doppler sonography. It is also possible to use three- and four-dimensional procedures (stic, live-3D) and multislice imaging sequences (TUI, i-slice). The aim is to prenatally diagnose and to improve the treatment of congenital heart defects. In order to be able to perform fetal echocardiography and anomaly diagnosis, the examiner must be particularly highly qualified and have enough relevant experience, and a high-resolution ultrasound scanner is required.

Bildtitel
The fetus at first trimester screening (3D)
Button
Bildtitel
Twins at first trimester screening (3D)
Button
Bildtitel
The fetus at mid gestation
Button
Bildtitel
The fetus 3D
Button
Bildtitel
Fetal face
Button
Bildtitel
Fetal face in late pregnancy
Button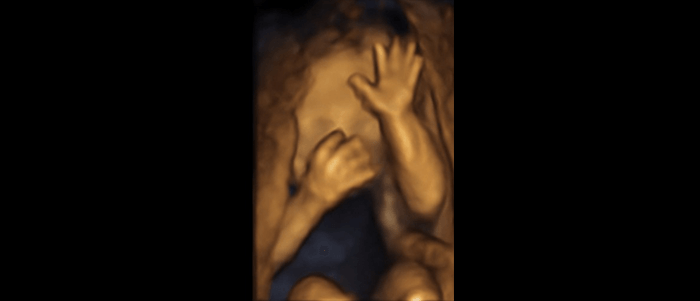
Bildtitel
The arms and hands 3D
Button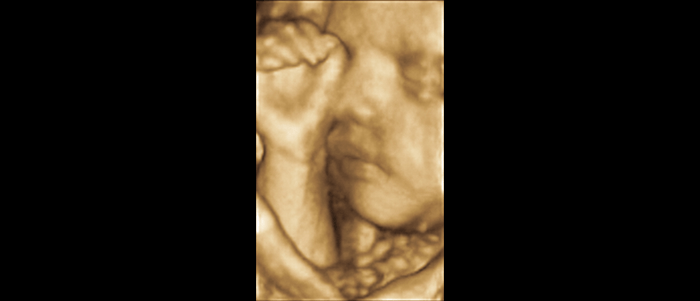
Bildtitel
Fetal face and one hand in front of the face
Button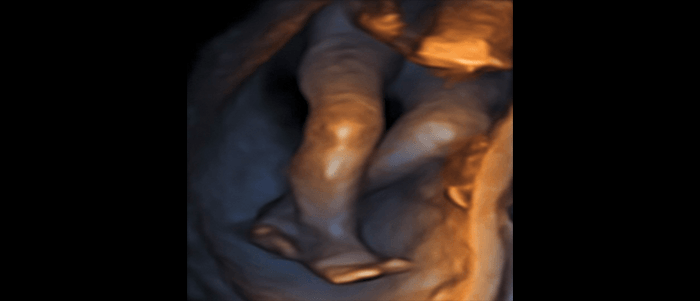
Bildtitel
The legs 3D
Button
Bildtitel
The feet 3D
Button
Bildtitel
Male genitalia
Button
Bildtitel
Spine
Button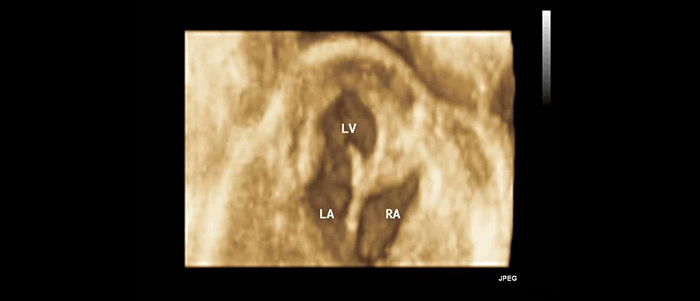
Bildtitel
3D echocardiography. Tricuspid valve atresia
Button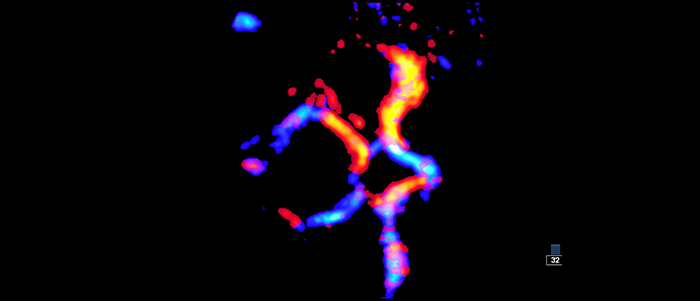
Bildtitel
Vessels of the fetal brain
Button
3D-4D-Ultrasound
3D Ultrasound permits a three-dimensional view of ultrasound findings. The ability to perform 3D ultrasound strongly depends on examining conditions (e.g., stage of pregnancy, amount of amniotic fluid, fetal position, thickness of abdominal wall)
Showing moving 3D images is known as 4D or Live 3D ultrasound.
PRÄNATALZENTRUM STUTTGART
Prof. Dr. med. Gunther Mielke & Dr. med. Stephan Bosselmann
Richard- Wagner-Str. 11 - 70184 Stuttgart
Tel. 0711 78 27 99 3 - Fax 0711 78 27 99 4
Mobile / Private consultation 0049 157 80 63 26 93
www.praenatal-ultraschall.de - praxis@praenatal-ultraschall.de